Do kids with substance use disorder have equal access to evidence-based care?
Opioid agonist treatments (i.e., methadone & buprenorphine) are evidenced-based protocols that have been shown to prevent overdose and increase remission rates, but do adolescents have equal access?
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Between 1992 and 2012, the prevalence of opioid misuse and opioid use disorder doubled among adolescents, although more recent trends are declining. Opioid agonist treatment (i.e., medicated assisted treatment or MAT) is a life-saving treatment for opioid use disorder that can prevent lethal overdose and reduce injection drug use. The effectiveness of opioid agonist therapies has been well investigated among adults but is less studied among adolescents. Recently, the American Academy of Pediatrics recommended that pediatricians consider opioid-agonist treatment for adolescents with severe opioid use disorders describing it as “underused” and “severely restricted.” This study aimed to fill the knowledge gap regarding the extent of opioid agonist treatment use among adolescents treated for opioid use disorder in the US and compare the results to adults.
HOW WAS THIS STUDY CONDUCTED?
This study used secondary data analysis from the 2013 Treatment Episode Data Set (TEDS), a federal database of state administrative records on substance use disorder treatment episodes that occur in publicly funded facilities. Participants data were included if they received opioid agonist treatment as defined by methadone or buprenorphine (but not naltrexone) to treat heroin, nonprescription use of methadone, or other opiates at a specialty treatment facility. Five states, and an additional 5.5% of the records, were excluded for not providing the data included in the analysis. The final sample included 139,092 first treatment episodes. Adolescents comprised 2.2% of the sample of episodes, including 1.1% of episodes of treatment for heroin use and 3.2% of episodes of treatment for all other opioids.
WHAT DID THIS STUDY FIND?
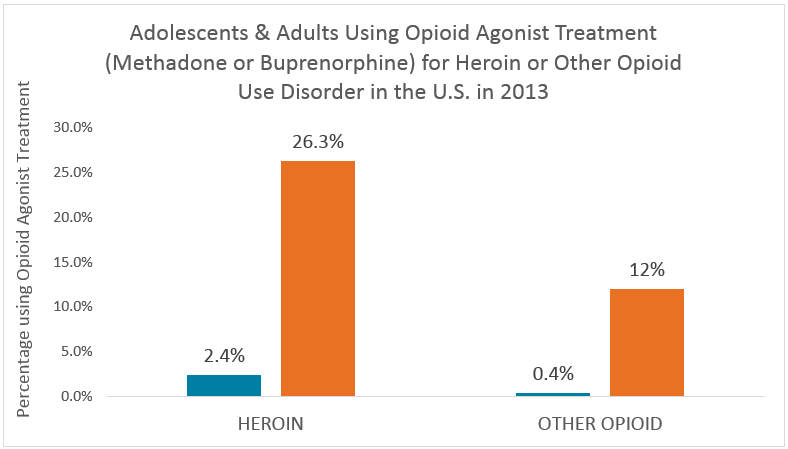
This study compared the proportions of adolescents and adults who received opioid agonist treatment by heroin use disorder versus other opioid use disorders. For heroin use disorder, 2.4% (n=18) of the 761 adolescents received opioid agonist treatment compared to 26.3% (n=17,380) of 66,074 adults. For patients with an other opioid use disorder, 0.4% (n=9) of 2,325 adolescents received opioid agonist treatment compared to 12% (n=8,363) of 69,932 adults (see figure below).
Other factors that could affect the likelihood of receiving opioid agonist treatment were also compared. Specifically, adolescents were less likely than adults to be homeless, were more likely to report using more substances at admission, and were more likely to be referred by the criminal justice system. For example, 40.8% of adolescents compared to 22.7% of adults in treatment for an other opioid use disorder were referred through criminal justice. After adjusting the comparisons between adolescents versus adults who receive opioid agonist treatment for confounding variables (i.e, gender, race-ethnicity, number of substances used, referral source, and housing status), the results remained highly similar.
WHY IS THIS STUDY IMPORTANT
Opioid use disorder is a lethal chronic health condition. Opioid agonist treatments can prevent cravings, mitigate withdrawal symptoms, and block the effects of other opioid drugs. The availability of opioid agonist treatments has changed the trajectory of the disorder resulting in fewer deaths, HIV infections, less drug use, and increased remission rates and improved quality of life. Among adolescents, opioid agonist treatment has been shown to be a helpful treatment for increasing remission rates.
This study has found that opioid agonist treatment is rarely used for adolescents and access to this treatment is highly restricted in the US. In general, adolescents and emerging adults have lower rates of treatment retention compared with adults, underscoring the need to deliver developmentally appropriate evidenced based protocols to improve health and quality of life.
- LIMITATIONS
-
- Office-based physicians were not included in the TEDS dataset but may provide buprenorphine; therefore, the percent of patients using opioid partial agonist treatments could be underestimated.
- Second, a measure of severity or health insurance may influence the likelihood of using opioid agonist treatments but these variables were not available and thus not accounted for in the comparative analysis between adolescents and adults.
NEXT STEPS
Future research should identify the barriers that restrict access to opioid agonist treatments for adolescents and adults and identify for whom opioid agonist therapies may be contraindicated.
BOTTOM LINE
- For individuals & families seeking recovery: This study found that only 2.4% of adolescents in treatment for heroin use disorder received opioid agonist treatment as compared to 26.3% of adults. Additionally, only 0.4% of adolescents in treatment for prescription opioids received opioid agonist treatment, as compared to 12.0% of adults. Opioid agonist treatments can prevent cravings, mitigate withdrawal symptoms, and block the effects of other opioid drugs; however, this study showed that access is highly restricted in the US. If you or someone you know are struggling with an opioid use disorder, be persistent in learning all your treatment options including opioid agonist treatments.
- For scientists: This study identified that only 0.4% of adolescents in treatment for prescription opioids received opioid agonist treatment, as compared to 12.0% of adults. Policies, attitudes, and messages that serve to prevent patients from accessing a medication that can effectively treat a life-threatening condition may be harmful to adolescent health. Additional research should focus on identifying any contraindications for adolescents’ use of opioid agonist therapies and identify the barriers to accessing opioid agonist treatments.
- For policy makers: This study shows that adolescents in specialty treatment for opioid use disorders rarely receive opioid agonist treatments. The American Academy of Pediatrics advocates for increasing resources to improve access to opioid agonist treatments for adolescents and young adults with an opioid use disorder. Regulatory changes and expansions of Medicaid coverage for opioid agonist treatments could improve access to evidence based treatments.
- For treatment professionals and treatment systems: This study found that adolescents in specialty treatment for either heroin or prescription opioid use disorders rarely receive opioid agonist treatments. This may reflect patient, parent, or provider preferences and concerns about the appropriateness of opioid agonist treatments for adolescents. Encourage your staff and patients to become informed about the clinical outcomes associated with opioid agonist treatments (i.e., prevent cravings, mitigate withdrawal symptoms, block the effects of other opioid drugs, prevent lethal overdose, and increase remission rates) so they can assemble a treatment plan that is evidenced based and the most likely to support recovery.
CITATIONS
Feder, K. A., Krawcyk, N., Saloner, B. (2017). Medicated-assisted treatment for adolescents in specialty treatment for opioid use disorder. Journal of Adolescent Health, June 60(6), 747-750.

