What types of individuals respond best to contingency management approaches?
Contingency management is an evidence-based treatment for substance use disorder (SUD) in which incentives (e.g., prizes, cash vouchers) are offered to patients in response to them successfully attending treatment sessions or remaining abstinent (generally verified though drug and/or alcohol testing) or otherwise achieving some other recovery-related behavior change. Contingency management, in general, consistently improves treatment attendance and abstinence rates; however, little is known about whether certain patients (younger or older patients, or those with greater SUD severity, etc.) do better than others in response to contingency management. This study describes results from a systematic review that examined such factors.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Contingency management is a standardized behavioral intervention that can be readily integrated into existing treatment programs and delivered by behavioral health professionals. However, contingency management is underutilized, largely due to concerns regarding a) available funding for contingency management treatment programs, and b) the element of chance in the rewards individuals might receive for abstinence or behavior change, which may resemble gambling and the potential for the creation of a new addictive problem.
The cost-effectiveness and long-term sustainability of contingency management programs are limited because results tend to vary quite a bit across different patients. As with any intervention for SUD, some patients that do in fact receive contingency management during outpatient treatment do not achieve improved abstinence relative to standard outpatient treatment alone. This study investigated patient-level characteristics that might be associated with greater or lesser contingency management benefits, with the hope that understanding such factors will help programs develop and deliver more effective individualized care that is better matched to patients’ needs.
HOW WAS THIS STUDY CONDUCTED?
This review article evaluated and summarized existing studies that examined individual difference factors in contingency management, focusing on individuals with stimulant (e.g., cocaine, meth/amphetamine) and/or opioid use disorder. Authors reviewed 39 studies that analyzed whether patient characteristics and/or treatment-related behaviors affected contingency management treatment response relative to a comparison group (e.g., individuals receiving treatment but without the additional contingency management).
Publications selected for inclusion: (1) reported a primary or secondary analysis testing for individual difference factors that either predicted or influenced the degree of derived benefit from contingency management, (2) reported a total sample comprised of ≥20 adult stimulant and/or opioid users treated in an outpatient setting, (3) evaluated a contingency management study in which stimulant and/or opioid abstinence was reinforced as a primary target behavior, and (4) evaluated individual difference factors in contingency management outcome against a “standard care” or low-dose contingency management (e.g., a contingency management approach with a very low reward for abstinence) control condition. Experimental implementations of contingency management (such as computerized-, online-, or group-based delivery of the intervention) were excluded from the review, as were programs offering nonmonetary/prize-based reinforcement (e.g., housing, employment, or treatment-related privileges). Contingency management programs reinforcing additional target substances or behaviors (i.e., beyond stimulant and/or opioid abstinence) were included, provided that stimulant and/or opioid abstinence was a primary focus of reported results.
WHAT DID THIS STUDY FIND?
Severity of substance use history and complexity of past experiences affect contingency management benefit.
This review examined the following factors: (1) motivation to change and substance use before and during treatment, (2) substance use comorbidity and chronicity, (3) psychiatric comorbidity and severity, (4) medical, legal, and sociodemographic variables, and (5) cognitive-behavioral variables. We will review each one briefly:
- Motivation to change and substance use before and during treatment. Motivation to change did not appear to affect the success of contingency management treatment, as studies found no differences between those reporting “high” vs “low” motivation for change. Patients receiving contingency management achieved longer durations of continuous abstinence compared to standard treatment, suggesting contingency management prolonged abstinence regardless of pretreatment motivation to change. However, individuals testing positive for targeted substances at the beginning of the treatment, and heavier users in general, had poorer outcomes from contingency management compared to those with negative screens and lighter users.
- Substance use comorbidity and chronicity. Use of more than one substance (e.g., cocaine use and opiate use, or cocaine use and alcohol use) did not detract from the success of contingency management. Also, a noteworthy finding – given the concerns about “games of chance” among those with prior gambling behavior and obvious addictive tendencies – was that the benefits of contingency management (i.e., reduced cocaine, opioid, and alcohol use and improved treatment retention) were comparable for patients with and without past month gambling behavior, and a significant reduction in gambling behavior at post-treatment was identified in contingency management recipients. Studies also found improved retention in treatment, and longer durations of abstinence, in contingency management for patients with two or more previous treatment episodes, suggesting that contingency management may be particularly beneficial in those with more severe clinical presentations. Age of onset of SUD did not appear to affect the benefits of contingency management with respect to duration of abstinence and treatment retention.
- Psychiatric severity and comorbidity. Patients consistently achieved improved outcomes (i.e., higher rates of prolonged abstinence) in contingency management relative to standard care, regardless of psychiatric symptom severity. Moreover, while patients with higher levels of psychiatric symptom severity show poorer retention in standard treatment, this was not the case with contingency management; in fact, those with greater symptom severity showed improved retention in contingency management. Unique benefits of contingency management have similarly been shown in patients with specific psychiatric diagnoses and risk factors (e.g., history of sexual abuse, history of major depressive disorder, or PTSD symptoms).
- Medical, legal, and sociodemographic variables. In general, these factors did not meaningfully impact contingency management treatment response. Specifically, income level (past month income), race/ethnicity, HIV status, history of trading sex for drugs or money, and current pregnancy did not influence the benefits of contingency management. Factors that were associated with greater benefit from contingency management were: being female, absence of current legal problems, and utilization of homeless or recovery-focused housing programs during treatment. While patients referred to treatment by the criminal justice system demonstrated improved outcomes overall, benefits of contingency management with respect to abstinence and retention were most pronounced in patients who were not referred by the criminal justice system. Whether age is a factor in the benefits of contingency management is unclear, with some studies finding greater benefits in younger patients, and others finding greater benefits in older patients.
- Cognitive-behavioral markers. Only one study examined individual differences in cognitive-behavioral performance in reference to contingency management treatment. This study found that individuals who like to take more risks in their lives generally achieved shorter periods of abstinence across contingency management treatment conditions, suggesting that perhaps larger rewards are needed in those who like to take more risks. There is also some evidence that cognitive-behavioral therapy can be combined with contingency management for better outcomes.
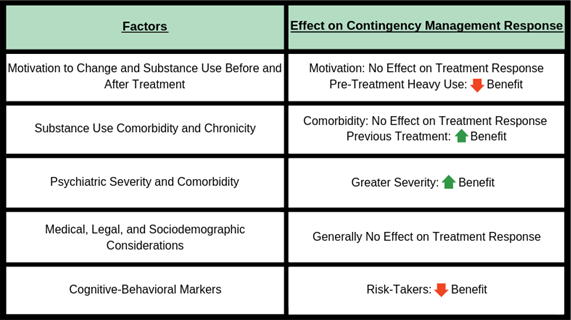
Figure 1. Sociodemographic and health factors and their impact on contingency management treatment response.
To summarize, factors associated with more severe and/or complex clinical presentations (i.e., testing positive for target substances at treatment entry, more previous treatment attempts, history of sexual abuse, diagnosis of antisocial personality disorder, failure to disclose ongoing cannabis use, history of major depressive disorder, current PTSD) were associated with increased benefits of contingency management. While there are strong indications that contingency management may be especially beneficial in the most severe cases, continued research is necessary to confirm and clarify these findings.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
In this review, contingency management was nearly always beneficial; contingency management was only rarely associated with no clinical benefit and rarer still with poorer outcomes when compared to not providing it. On the whole, evidence suggests that contingency management may be especially beneficial in patients who might otherwise have poorer outcomes (for example, those who test positive for targeted substances at treatment entry, patients with more previous treatment attempts, and those with antisocial personality disorder). However, differing aspects of contingency management may be necessary to achieve these benefits (e.g., higher reinforcement magnitude and reinforcement schedules that encourage early retention) and these requirements may also intersect with patient-level characteristics, such as age, race, or psychiatric comorbidity. Patients expected to have better outcomes may, correspondingly, exhibit less pronounced benefits of contingency management due to a ceiling effect (e.g., further improvement is not possible due to high levels of abstinence in standard care or among those involved in the criminal justice system who already have high external oversight and monitoring). This is important, as other studies have also suggested that contingency management may be a cost-effective clinical strategy to reduce stimulant use among individuals with stimulant use disorders and serious mental illness, which can be a challenging population. Therefore, contingency management is likely beneficial and cost-effective.
- LIMITATIONS
-
- Nearly all of the studies included in this review were secondary analyses of existing datasets not specifically designed to test individual-level factors that might influence contingency management success. Therefore, much of the data were derived from standard intake assessments commonly used in clinical trials, rather than targeted questions. Consequently, very little prior work has been conducted designed specifically to investigate predictors of contingency management response.
- The majority of previous research in this area has been conducted by a single research group and has often utilized the same primary data sources for secondary analyses. To address these limitations, future work should focus on replication by other investigators in other treatment samples to see if results hold.
- Many of these studies were small, so results should be replicated in larger samples.
BOTTOM LINE
- For individuals and families seeking recovery: This review showed that individuals in treatment for substance use disorder (SUD) can benefit from contingency management interventions. Further, those who benefit the most may be the most severe or complicated patients, such as those with greater psychiatric severity or comorbidity. Contingency management in combination with additional treatments (medication, therapy) may work best. As contingency management is not widely integrated into addiction treatment, patients and their families may want to speak to their treatment providers about availability of contingency management interventions.
- For scientists: Despite the clear potential for individual difference factors to inform precision implementation of contingency management, relatively little research has been conducted to advance this aim. The majority of findings resulted from secondary analysis of previously-collected datasets, which has constrained the breadth of patient-level data available for consideration. For example, while most publications focused on variables that are commonly evaluated in clinical trials (e.g., demographics, clinical diagnoses, symptom severity), only one study involved a hypothesis-driven cognitive-behavioral measure. Furthermore, the majority of previous work (comprising 64% of included publications) was conducted by a single research group and nearly half of included data were pooled from the same three early trials of contingency management in opioid and/or cocaine users. For these reasons, generalizability remains a potential concern. Thus, this research supports the need for more studies investigating hypothesis-driven predictors of contingency management treatment response, such as theoretically-informed psychometric, genetic, and/or neurobiological markers. Also, more work is needed to determine optimal durations of contingency management sufficient to support long-term change and remission. Finally, the question of why the more severe patients had greater beneficial response to contingency management is intriguing. Future studies could attempt to further unpack this relationship by asking questions of whether more severe groups value rewards more (for instance, if they have less financial resources/recovery capital), or whether these groups have greater motivation because of greater severity.
- For policy makers: Despite evidence that individuals in treatment for substance use disorder (SUD) can benefit from contingency management interventions, contingency management remains underutilized – due in part to concerns regarding available funding for contingency management treatment programs. Policy-maker collaborations with treatment professionals and scientists to develop policies and regulations concerning contingency management treatment may improve patient outcomes while reducing costs over the long-term. This article indicates that contingency management may be most beneficial the more severe or complicated the patients. Policy-makers might also consider steps to reimburse this treatment, especially for patients with complicated histories.
CITATIONS
Forster, S. E., DePhillippis, D., & Forman, S. D. (2019). “I’s” on the prize: A systematic review of individual differences in Contingency Management treatment response. Journal of Substance Abuse Treatment, 100, 64-83. doi: 10.1016/j.jsat.2019.03.001

