Automated contingency management using smartphones may reduce barriers and improve opioid use disorder treatment
Contingency management is among these most effective interventions for many types of substance use disorders. Barriers to its implementation, however, reduce the likelihood that treatment programs will adopt this empirically supported intervention. In this study, researchers evaluated the acceptability and effectiveness of an automated contingency management smartphone application to improve opioid use disorder (OUD) treatment.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Despite compelling evidence supporting the effectiveness of contingency management for many types of substance use disorders, key barriers to adoption include negative, often incorrect, beliefs and biases about its efficacy, and costs. Automation of contingency management using smartphone applications provides a means of circumventing barriers to implementation, such as provider beliefs, training levels, limited provider time (e.g., of training and implementation), and can be used as add-ons to standard care. At the same time, there is little information about these automated contingency management interventions, and a need to evaluate their use and efficacy for OUD treatment. These researchers sought to address this knowledge and service gap by conducting a pilot study to evaluate the efficacy and acceptability of an application that incentivized abstinence from opioids and other drugs, adherence to the OUD medication buprenorphine, as well as treatment session attendance during outpatient OUD treatment.
HOW WAS THIS STUDY CONDUCTED?
This study was a non-randomized pilot trial of an automated contingency management application plus standard outpatient care, compared to standard care among patients in another nearby outpatient clinic (control condition). Both inner-city substance use disorder clinics provided outpatient, intensive outpatient, and continuing care treatment to patients with OUD. The researchers compared outcomes of their app-based intervention by matching participants in their study with patients from the nearby clinic. Specifically, the researchers matched individuals in the treatment condition to individuals at the other clinic (the control condition) by first selecting patients who entered treatment on the same day, had a urine test on or before the day the participant in the treatment condition started using the app, enrolled in the same level of care (e.g., outpatient, intensive outpatient), and had the same primary diagnosis of OUD. This matching strategy worked for all but eight participants in the treatment condition, who were subsequently removed from the analysis, resulting in 85 matched pairs (N = 170).
For 4 months, the application was used as an add-on to standard care, which included individual and group counseling, medication (e.g., buprenorphine), onsite urine testing, and optional paper-and-pencil Cognitive-Behavioral Treatment (CBT) materials (e.g., worksheets). Usability and acceptability, which included measures of how usable the platform was and participants’ likelihood of recommending it to a friend, was assessed during post-pilot study focus group meetings. The researchers also examined abstinence and use of medication for OUD (as measured by urine toxicology results), treatment attendance, and intervention acceptability and satisfaction.
The application was designed to deliver financial incentives for consistent abstinence from drugs, persistent use of medications for OUD (i.e., buprenorphine), verified attendance at scheduled (i.e., clinic-based) and optional treatment (mutual help groups), and use of CBT modules within the app.
For contingency management, participants could earn up to $100 per month for providing recovery-consistent urine results (i.e., abstinence and evidence of buprenorphine adherence, as confirmed by clinic) and treatment attendance (measured by GPS, confirmed by clinic staff), and an additional $1 for each CBT module completed (i.e., up to $36). GPS was used in this study, which included the same technology as “maps” applications on smartphones, to determine whether the participant was present at the treatment facility. Monetary incentives were transferred to patients’ reloadable Visa smartcards, which blocked cash withdrawals and limited expenditures to prevent suspect purchases or use at bars, liquor stores, casinos, etc.
Participants included 85 matched pairs, for a total of 170 participants. All participants had an OUD (diagnosed at clinic intake), while half of the study participants were women (51%) and 61% were White/Caucasian. Participants were 38 years old on average (SD = 9.5). The participants in the treatment and comparison group were similar on all measured domains, with the exception of individuals in the intervention group having a higher percentage of prescribed buprenorphine use.
WHAT DID THIS STUDY FIND?
Patients with OUD who received automated contingency management via the app were more likely to provide abstinent/medication adherent urine results for the duration of the study. These patients also reported significantly higher rates of scheduled session attendance.
Users of the contingency management intervention reported a high level of acceptability and satisfaction with the intervention, including on measures of whether they would refer a friend to use the app and overall satisfaction. The researchers also noted that of the 13 participants who left treatment prematurely and returned, each requested to use the application again. The clinic staff reported that the overall burden of the intervention was “negligible,” requiring little to no time or effort on the part of providers. The researchers stated that anecdotally, CBT module usage was greater with the app than in standard care, using the paper-and-pencil CBT content.
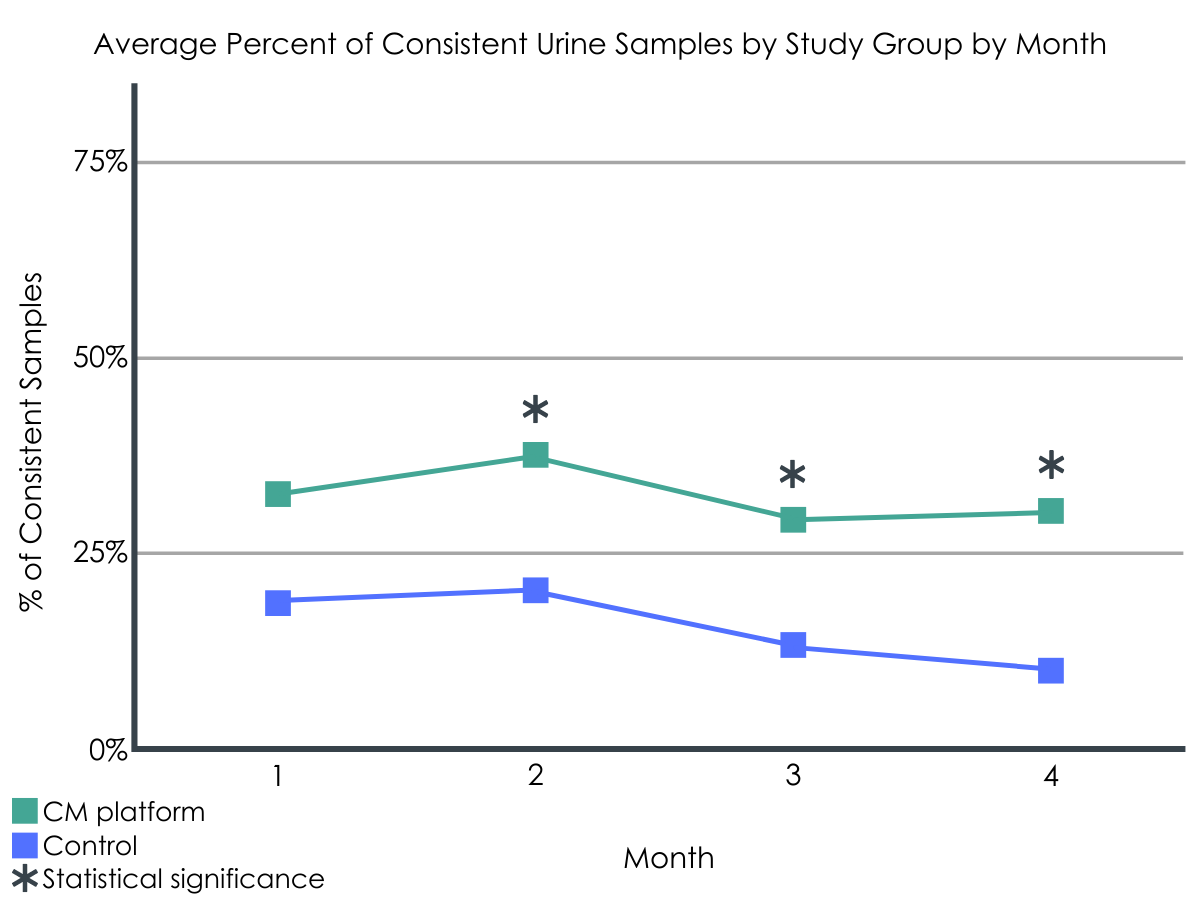
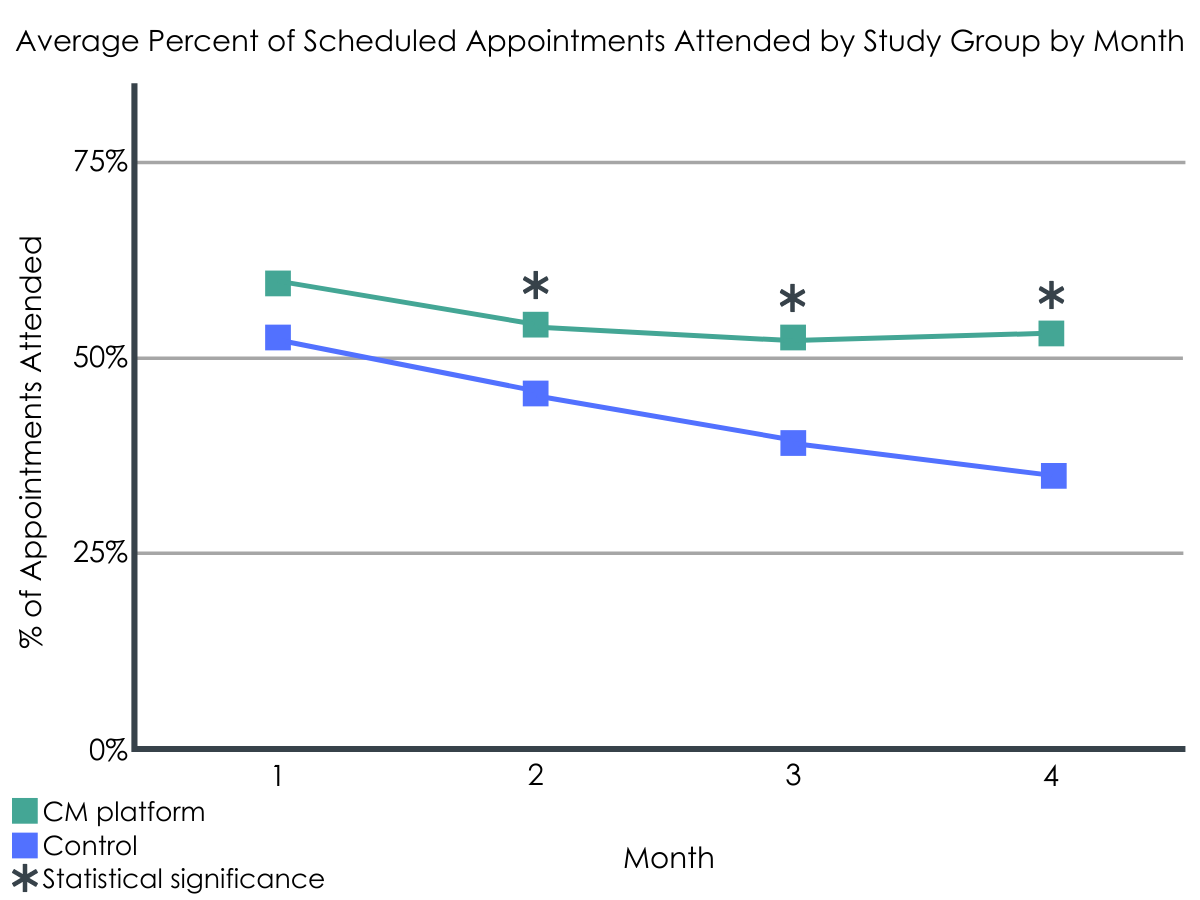
Figures 1 and 2.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Automation of contingency management and delivery via smart phone applications appears to be acceptable to patients and is associated with higher rates of abstinence/medication adherent urine results and treatment attendance compared to standard outpatient care. Importantly, the researchers stated that their incentives were lower than in comparable studies, which could have reduced the observed group differences among patients. It is possible that effects would have been more pronounced with larger incentives. In either case, automation and ease of implementation of app-based contingency management may circumvent key implementation and procedural barriers, including logistical constraints, fidelity of and timely reinforcement, and lack of provider training, or other attitudinal biases that might otherwise limit the adoption of efficacious contingency management.
Contingency management is most often applied to target one or two circumscribed target behaviors, such as consistently negative urine toxicology results or treatment attendance. The approach in the current study was to target these behaviors, as well as engagement in the CBT modules of the app, and participation in additional interventions (mutual help group attendance) of their choosing. This approach resulted in significant improvements on several target behaviors, including both therapy process behaviors (treatment session attendance, which is associated with improved recovery outcomes) and outcomes (urine toxicology results). Although the study used a matched control condition and did not use a more scientifically rigorous randomized design, the findings remain suggestively compelling. In addition, the reported acceptability and satisfaction among app users provides further evidence of the potential utility of automated contingency management to supplement standard outpatient treatment for OUD.
- LIMITATIONS
-
- Participants were not randomized and comparisons between conditions were made between patients being treated at different facilities. While the two groups were similar on most measured characteristics, increasing confidence the advantage for the CM smartphone intervention was indeed due to the intervention itself, participants could have differed on other unmeasured characteristics. For example, there might have been important differences between the clinicians, services offered, or other factors unique to each site.
- The application used and evaluated in this study was considered an add-on to standard care and was not used in an integrated fashion with standard care.
- The researchers made two modifications to the intervention during the study; the first was that they limited the number of optional sessions patients could be compensated for, and also increased the number of CBT modules from 36 to 90. These modifications have unknown implications for study findings but are noted in light of possible effects on the observed outcomes.
BOTTOM LINE
Contingency management involves providing timely incentives to individuals for health behavior change, such as treatment engagement and illicit opioid abstinence. The results of this study support the notion that automated contingency management, provided via a smartphone application, can help improve treatment attendance and lead to higher rates of abstinence/medication adherent urine results.
- For individuals and families seeking recovery: These results provide further support for the effectiveness of contingency management for patients with OUD, which individuals and families might consider pursuing to support recovery from OUD. The application used in the current study, provides some preliminary “proof of concept” data that app-based electronically delivered financial incentive contingency management may improve important near-term clinical outcomes. However, contingency management is more often delivered currently by providers within clinics.
- For treatment professionals and treatment systems: Contingency management is an effective intervention for opioid use and other substance use disorders. Expanding the use of contingency management within clinics could improve outcomes for outpatients with OUD. In addition, supplementing standard care with app-based contingency management could potentially lead to improved patient outcomes, while also circumventing barriers to providing in-person continency management.
- For scientists: This study was described as a pilot trial of an app-based contingency management intervention design to incentivize treatment attendance, engagement in CBT-based app content, and consistent negative urine toxicology results. Outcomes of pilot trials should be interpreted with caution, and some advocate that they should not be used for hypothesis testing. As such, findings from this study would benefit from replication. It would be beneficial for follow up research to be fully powered, and to employ randomization to overcome limitations with participant matching between separate outpatient clinics, as was done in the current study. Future studies might benefit from follow up analyses to examine the degree to which engagement with the app, or adherence, are associated with improvements on primary outcomes, or test a care delivery model wherein use of the app is integrated with standard care (e.g., provider introducing the application and checking in to monitor use, adherence, and perceived effectiveness). Future research might also follow additional app development to further customize the intervention; tailor content, delivery, and contingencies, target behaviors, and magnitude of the incentives/rewards to individual patients; and evaluate the optimal duration of incentive delivery to promote sustained recovery.
- For policy makers: Contingency management is an efficacious and cost-effective intervention for substance use disorder. Further, the results of this study suggest that apps can be designed to provide automated contingency management. The app used in the current study was associated with improved treatment attendance and rates of negative urine toxicology screens. This automated application of contingency management provides important implications for future implementation and scalability of this intervention for wide-spread use and adoption. However, to be successful, it would be beneficial to increase funding and policy support for the development, implementation, and dissemination of contingency management interventions. It might also be especially helpful for policy makers to consider models for reimbursing contingency management services and increase access among patients who might not otherwise have the means to participate in this type of intervention. Another important consideration is that it is not yet known what the optimal incentive delivery duration is for patients. Additional research could help to clarify this question to ensure that contingency management is delivered for a sufficient duration.
CITATIONS
DeFulio, A., Rzeszutek, M. J., Furgeson, J., Ryan, S., & Rezania, S. (2021). A smartphone-smartcard platform for contingency management in an inner-city substance use disorder outpatient program. Journal of substance abuse treatment, 120, 108188. doi:10.1016/j.jsat.2020.108188

