Strategies to reduce alcohol harms may be more effective for some than others: A focus on mental health
Protective behavioral strategies are tools that an individual can use to limit harms related to the amount of alcohol one uses when in situations where alcohol is likely to be present (for example, when at a party). This study examined whether the use of protective behavioral strategies predicted the amount of alcohol consumed and alcohol-related consequences among young men in Switzerland. It also explored whether having a mental health condition influenced the relationship between the use of protective behavioral strategies and alcohol-related outcomes.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Protective behavioral strategies are cognitive-behavioral tools that an individual can use to limit the amount of alcohol one drinks, and the harms alcohol consumption might cause, and thereby potentially reduce alcohol-related consequences when in situations where alcohol is likely to be present. For example, when at a party with friends, an individual could use the protective behavioral strategy of drinking a full glass of water between every alcoholic beverage. Some research indicates that protective behavioral strategies can be effective in reducing alcohol use and related consequences, yet it is not clear that these strategies work for everyone, or that everyone uses them in the same way.
Some research suggests that although individuals are capable of learning these strategies, they may not actually utilize them in a social situation depending on the characteristics of the social situation and individual underlying characteristics. Also noteworthy is that individuals who use alcohol as a way to cope with unpleasant or distressing emotion (i.e., “drinking to cope”) are more prone to experiencing drinking-related problems.
This study examined whether the use of protective behavioral strategies predicted the amount of alcohol consumed and alcohol-related consequences among young men in Switzerland. To focus specifically on individuals who might be more prone to drinking-related problems, and therefore deserve more focused attention, the research team also explored whether having a mental health condition, such as depression, bipolar spectrum disorder, borderline personality disorder, or social anxiety disorder, influenced the relationship between the use of protective behavioral strategies and alcohol-related outcomes.
HOW WAS THIS STUDY CONDUCTED?
The data were collected from a sample of young men through army recruitment centers in Switzerland through the “Cohort Study on Substance Use Risk Factors”. In Switzerland, a large majority of the male population must go through the recruitment process of the Swiss army (approximately 98% of Swiss 18-year-old males). The study collected three waves of data starting with a young male cohort in 2010-2011 (age 18-19 years), followed by a re-assessment in 2012-2013 and a third assessment in 2016-2017. Data were collected in French and German, depending on the Swiss region of recruitment. The total study sample was 7,556 and the analytic sample used in this study was 4960 males from the second assessment (2016-2017). Therefore, while the data were obtained from a longitudinal study (multiple assessment points over time), this study was cross-sectional because the variables came from a single assessment.
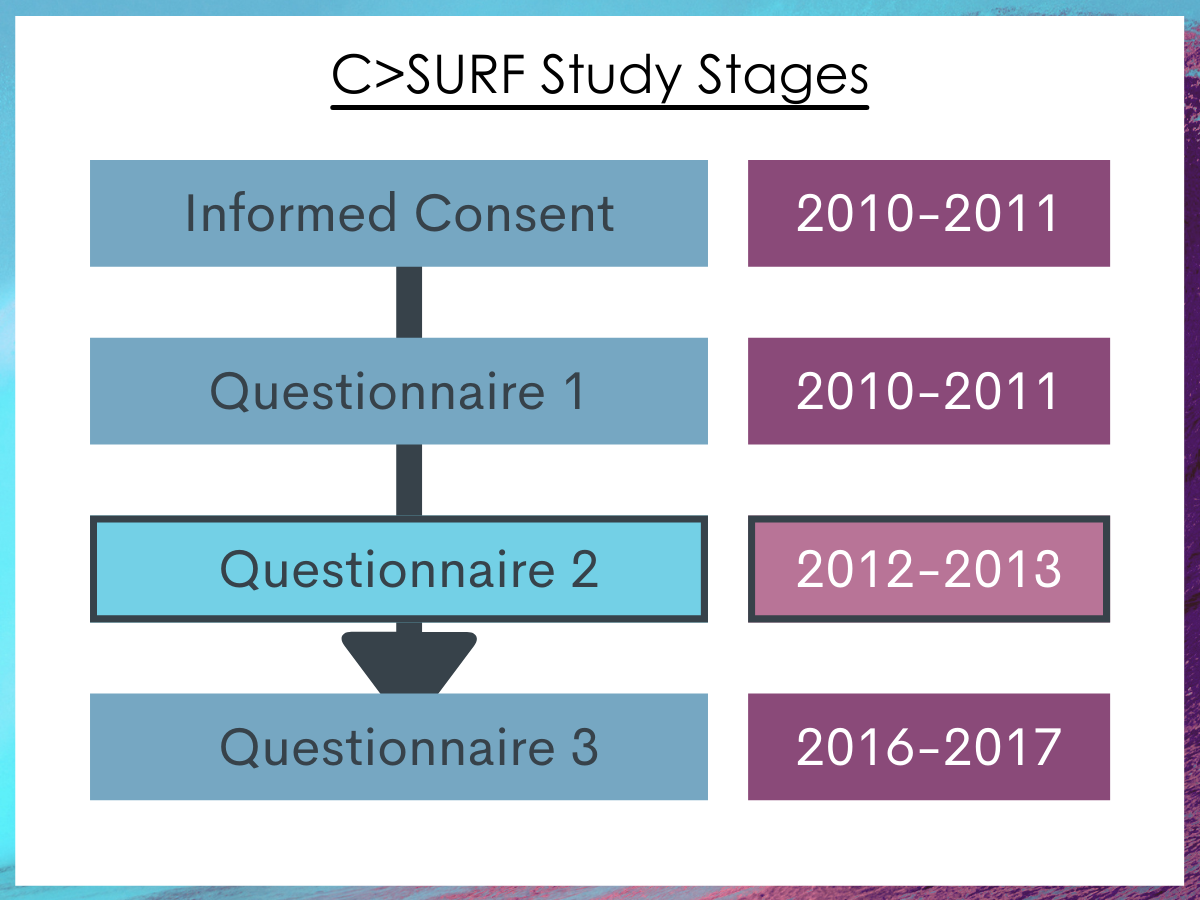
Figure 1. The data for this paper was taken from the second assessment wave (questionnaire 2) of the Cohort Study on Substance Use Risk Factors (C>SURF).
The primary predictor was the use of protective behavioral strategies as measured by the 20-item protective behavioral strategies scale. The scale has 4 subscales: Manner of drinking, serious harm reduction, limiting stopping drinking (mixing nonalcoholic drinks with alcohol), and limiting stopping drinking (planned limits on drinking).
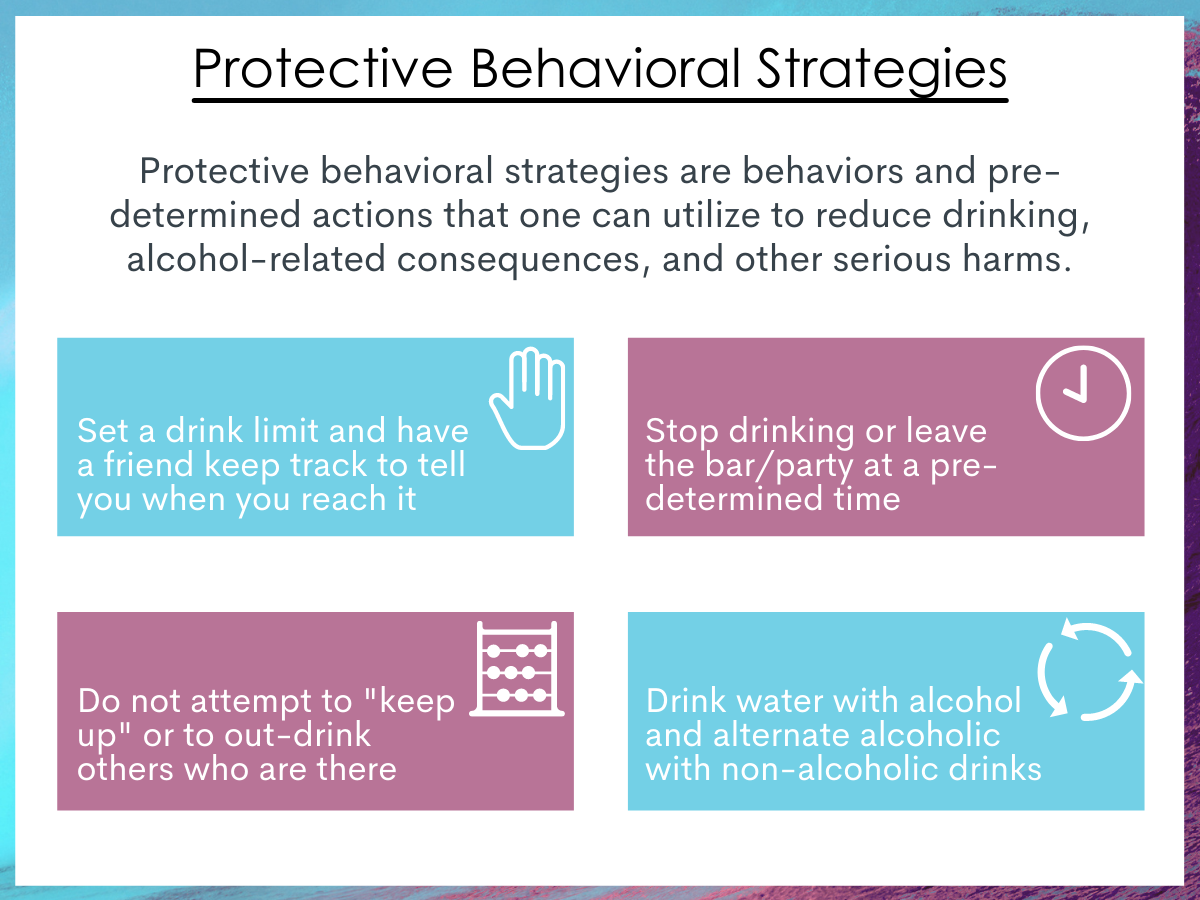
Figure 2. Examples of common protective behavioral strategies.
The primary outcomes were alcohol use measured in the number of drinks consumed each week and a summary score of the number of alcohol-related consequences (9 items total; e.g., getting in trouble with the police, having unplanned sex). The following are mental health conditions they examined as moderators: depression, bipolar spectrum disorder, borderline personality disorder, and social anxiety disorder. These mental health conditions were determined with several different standardized tools to assess whether a participant met the DSM-IV criteria for each condition.
The authors first examined correlations between all variables, then tested a series of statistical models separately for each mental health diagnosis that tried to control for several confounders (age, education, and linguistic region). The models used a stepped approach; in Step 1, each outcome was examined in relation to protective behavioral strategies and mental health diagnosis and in Step 2, the interaction between mental health diagnosis and protective behavioral strategies was added. These interactions examined whether the association between protective behavioral strategies and drinking outcomes were different for those with and without each of the mental health diagnoses that were assessed for by the research team.
The overall protective behavioral strategies score and its subscales were used in the analysis in separate models. Because one would expect more drinking to result in more alcohol-related consequences, the number of drinks consumed each week were included in the model examining alcohol-related consequences as another control variable (i.e., in addition to the other control variables age, education, and linguistic region) to better identify the moderation effects of mental health diagnosis.
The study sample included 4960 male participants who were on average 25 years old, majority French speaking (57%; versus German speaking), and who did not report abstaining from alcohol. They were all recruited from the Switzerland Army Recruitment Centers, a mandatory process for all young adult Swiss males.
WHAT DID THIS STUDY FIND?
Protective behavioral strategies were associated with fewer drinks consumed weekly.
The protective behavioral strategies score (both the total and the subscales) were significantly associated with consuming fewer drinks; those who scored higher on the scale, indicating more use of protective behavioral strategies, were likely to consume fewer alcoholic beverages than those who scored lower on the scale (r = -0.15). The total protective behavioral strategies score was also associated with significantly fewer alcohol-related consequences (r = -0.13).
Having a mental health diagnosis of bipolar spectrum disorder or borderline personality disorder was associated with consuming more drinks each week.
Individuals with a bipolar spectrum disorder or borderline personality disorder were significantly more likely to consume more drinks (r = 0.04 and r = 0.05, respectively). Individuals with depression or social anxiety disorder did not drink significantly more alcoholic drinks each week (r = 0.02 and r = 0.01).
Having a mental health diagnosis of depression, bipolar spectrum disorder, or borderline personality disorder was associated with more alcohol-related consequences.
All mental health diagnoses were significantly associated with more alcohol-related consequences (correlations ranged from 0.06-0.12).
Moderation models indicated strong differences for individuals with borderline personality disorder.
Individuals with borderline personality disorder demonstrated stronger relationships between higher protective behavioral strategies score (total and subscales) and lower alcohol use, suggesting that protective behavioral strategies might be used effectively among this group to limit alcohol consumption. There was not, however, a similar moderation effect on alcohol-related consequences, indicating that although there was a relationship between reducing alcohol consumption and use of protective behavioral strategies among individuals with borderline personality disorder, this relationship did not extend to reductions in alcohol-related consequences.
Moderation models indicated some differences for individuals with depression.
For individuals with depression, there were several differences in the relationship between certain protective behavioral strategies and drinking outcomes. The protective behavioral strategies subscale, limiting stopping drinking (mixing nonalcoholic drinks with alcohol), was related to more drinks among individuals with depression. It is possible, then that this strategy may be have been less successful in reducing total drinks consumed for individuals with depression.
Moderation models indicated some differences for individuals with bipolar spectrum disorder.
For individuals with bipolar spectrum disorder, there were mixed findings between the use of certain protective behavioral strategies and alcohol outcomes. That is, those without bipolar spectrum disorder had a stronger association between the total use of protective behavioral strategies and alcohol-related consequences, suggesting that those who used protective behavioral strategies and were not diagnosed with bipolar spectrum disorder had fewer alcohol-related consequences. Alternatively, the use of protective behavioral strategies from the subscale, “manner of drinking”, was significantly related to more consequences for individuals with bipolar spectrum disorder.
Moderation models demonstrated few differences for individuals with Social Anxiety Disorder.
Individuals with social anxiety disorder did not demonstrate significant differences in drinking-related outcomes from those without social anxiety disorder except on the protective behavioral strategies subscale, “limiting stopping drinking-planned limits on drinking”, where they demonstrated more drinking.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Research has supported the use of protective behavioral strategies to reduce risky alcohol consumption, but there is a lack of understanding on how effective the use of these strategies are for different subpopulations. This study highlights the complexity of mental health, alcohol use, and strategies to reduce alcohol use. First, the authors found that having a mental health diagnosis of depression, borderline personality disorder, bipolar spectrum disorder, or social anxiety disorder was associated with increased alcohol-related consequences and that having a mental health diagnosis of depression, borderline personality disorder, or bipolar spectrum disorder was associated with increased alcohol use. Similarly, and in line with existing research, the use of protective behavioral strategies was associated with less alcohol consumption and fewer alcohol-related consequences, findings that support the use of protective behavioral strategies as a tool to limit excessive alcohol drinking and reduce alcohol-related consequences.
Importantly, the research team used data collected at one point in time (i.e., the study was cross-sectional). We cannot say, then, that use of protective behavioral strategies was responsible for reduced drinking or consequences. It is possible that, although these two variables are related, another variable, such as attention to health and well-being, is responsible for lower drinking and use of protective behavioral strategies. That said, in other longitudinal research, protective behavioral strategies have been linked with alcohol consumption such that increased use of strategies leads to decreased drinking and consequences.
One unique finding in this study came from the analyses that examined subgroups of individuals with and without mental health conditions. These findings suggest that the use of protective behavioral strategies may not work as a tool for everyone to reduce drinking and/or alcohol-related consequences. That is, protective behavioral strategies do not appear to equally benefit men with social anxiety disorder, depression, or bipolar spectrum disorder, while they may be highly beneficial for men with borderline personality disorder. Similarly, certain sets of protective behavioral strategies may not be similarly effective for all individuals; this study indicates that men with depression who use the limiting stopping drinking by mixing nonalcoholic drinks with alcohol strategy may still drink more than those without depression. As well, men with social anxiety disorder who used the protective behavioral strategy limiting stopping drinking by planned limits on drinking also drank more than those without social anxiety disorder.
- LIMITATIONS
-
- As detailed in the Implications section above, the study uses cross-sectional data which rules out making causal statements between use of protective behavioral strategies, mental health, alcohol outcomes. Yet, the general pattern of findings is theoretically consistent and show similarity to other longitudinal study findings in this area.
- It is not clear if participants had comorbid alcohol use disorder (in addition to their mental health diagnosis) or if individuals had comorbid mental health conditions (e.g., both borderline personality disorder and bipolar spectrum disorder); the findings may not generalize to individuals with these characteristics.
- The sample is entirely a young male army recruitment sample, so is not generalizable to females or to older populations.
BOTTOM LINE
In this study, researchers used data from one assessment period in a large cohort study in Switzerland to examine the relationship between the use of protective behavioral strategies and alcohol use and alcohol-related outcomes among young men. They also explored whether certain mental health conditions moderated the use of protective behavioral strategies and alcohol outcomes. Although they found, overall, that the use of protective behavioral strategies was linked to less alcohol use and fewer alcohol-related consequences, these findings did not universally translate to those with mental health conditions. That is, protective behavioral strategies do not appear to equally benefit men with social anxiety disorder, depression, or bipolar spectrum disorder, while they may be more beneficial for men with borderline personality disorder. Certain subsets of protective behavioral strategies were also not similarly effective for all individuals, suggesting that although they are a set of protective behavioral strategies, some strategies may be more (or less) effective for different groups of people.
- For individuals and families seeking recovery: The reduction of problematic alcohol use can result in improved health and cognition and reduced negative alcohol-related consequences. Thus, although abstinence from alcohol may be the safest option, the use of protective behavioral strategies may be an effective way to reduce problematic drinking. Specifically, planning ways to engage in less risky drinking may be highly effective in social situations. Yet, for individuals with additional mental health conditions, protective behavioral strategies may not result in the same outcomes as those without mental health conditions and alternative strategies may be needed. Having a discussion with your care team and support network may help you or your loved one discover effective strategies to reduce alcohol use and associated consequences in social situations.
- For treatment professionals and treatment systems: This study indicates the importance of understanding potential mental health comorbidities among individuals seeking to reduce their drinking, or among those who are experiencing alcohol-related problems but may not wish to seek out addiction treatment or have other barriers to treatment. This study also demonstrates how a one-size-fits-all approach will not work for reducing problematic alcohol use and that alternative methods to cognitive-behavioral strategies like protective behavioral strategies to address hazardous/harmful alcohol use may be needed for those with certain mental health comorbidities. Brief interventions may be particularly effective, especially during an initial meeting as a form of screening and referral to additional treatment or to address initial treatment barriers.
- For scientists: This study advances the burgeoning science of our understanding of specific cognitive and behavioral tools to reduce drinking by examining strategies used by individuals with and without mental health conditions. Although many of the alcohol use findings did not extend to alcohol-related consequences, the sample had a high proportion of zero reported alcohol-related consequences (51%) indicating that even heavy use may not be prolonged enough to result in severe alcohol-related outcomes; future research should include the length of time since drinking initiation in analyses examining alcohol-related consequences. As well, future longitudinal research that examines changes in alcohol trajectories over time and for specific types of drinkers (along with other individual-level characteristics) is necessary to fully understand mechanisms of behavior change for individual alcohol use.
- For policy makers: The reduction of problematic alcohol use can result in improved health and cognition and reduced negative alcohol-related consequences. Although abstinence from alcohol may be the ideal for those using alcohol compulsively, the use of protective behavioral strategies may be an effective way to reduce problematic alcohol use. Yet, these strategies do not appear to work for everyone. Funding which allows for further examination of which strategies work for which individuals and in what contexts, as well as funding which addresses gaps in the prevention, intervention, and referral to treatment pipeline should enable better determination of how best to address mechanisms of behavior change. Some of this research funding could specifically focus on public health messaging shown to affect change (e.g., Drinking a glass of water between alcoholic drinks).
CITATIONS
Grazioli, V. S., Studer, J., Larimer, M. E., Lewis, M. A., Bertholet, N., Marmet, S., . . . Gmel, G. (2020). Protective behavioral strategies and alcohol outcomes: Impact of mood and personality disorders. Addictive behaviors, 112, 106615. Doi: 10.1016/j.addbeh.2020.106615

