Buprenorphine versus extended-release naltrexone: A focus on individuals experiencing homelessness
For individuals with opioid use disorder, initiation of the medication buprenorphine may be easier than use of the extended-release naltrexone medication because the latter requires a period of complete abstinence which can be challenging to achieve and an unpleasant experience. Yet, some individuals might benefit more, or in different ways, by using extended-release naltrexone as it requires only a monthly injection whereas individuals must take buprenorphine daily. In this study, researchers focused specifically on individuals experiencing homelessness given the challenges they might face with daily medication adherence to examine whether and how they might benefit more from an extended-release medication for their opioid use disorder. Studies like these are key to better understanding recovery for vulnerable groups with unique needs.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Medications for opioid use disorder improve opioid use outcomes while substantially reducing the risk of overdose and death. Yet, research demonstrates that not all medications are effective for the same populations, potentially due to initial barriers with initiating these medications and other barriers around treatment adherence. For example, the injectable extended-release naltrexone (often referred to by the brand name “Vivitrol”) produces similar outcomes to buprenorphine (often prescribed in formulation with naloxone and known by the brand name “Suboxone”) for individuals who are able to initiate it. Specifically, initiating extended-release naltrexone can be challenging as it first requires a detoxification period from all opioids. Alternatively, buprenorphine requires a daily pill or film and does not need a complete period of abstinence before initiation. While buprenorphine is easier than extended-release naltrexone to initiate, its daily dosing requirement can be a major challenge. First, daily medication requires that one remembers to administer, and has access to their supply of, medication, a known barrier to medication treatment in many chronic health conditions. Furthermore, there may be other differences between the different medications and patient outcomes. For example, if patients present with additional symptoms or behavior that could get in the way of their recovery and that the medication can successfully target (e.g., depressive symptoms), then there may be additional reasons for some individuals doing better (or worse) than other individuals with different forms of medication.
Individuals with opioid use disorder who are also experiencing homeless are a population with unique treatment and recovery needs. A previous study showed that for individuals with opioid use disorder, the group assigned to receive buprenorphine had lower rates of relapse – 4 consecutive weeks or 7 consecutive days of opioid use – than the group assigned to receive extended-release naltrexone monthly injections. While the medications produced similar outcomes for those who successfully initiated treatment, fewer actually received the extended-release naltrexone to which they were assigned. Given the challenges of experiencing homelessness and recovery, in this study, the research team re-evaluated that study’s data to examine whether these individuals also benefitted more from buprenorphine. The research team also sought to explore differences in key potential pathways by which this group may have responded differently to treatment compared with individuals who were not experiencing homelessness.
HOW WAS THIS STUDY CONDUCTED?
This was a secondary analysis of the Extended-Release Naltrexone vs. Buprenorphine for Opioid Treatment (X:BOT) study data from a 24-week open label, randomized controlled trial among individuals with opioid use disorder who presented for inpatient treatment. Both groups received different medications: Of the 570 participants, one group of 283 participants was assigned to receive extended-release naltrexone via intramuscular injection every 28 days while the other group of 287 participants was assigned to receive a daily dose of buprenorphine–naloxone pill (dispensed to participants with a several week supply for participants to self-administer). The participants were recruited from the 8 community addiction treatment study sites that were part of the National Drug Abuse Treatment Clinical Trials Network (CTN) from 2014 to 2017.
The primary outcome in the analysis was return to use of opioids during the period 20 days after randomization to treatment condition and at the end of the 24-week trial. Return to use was defined as use of non-study opioids at least once a week for 4 consecutive weeks or at least daily for 7 days in a row. The key grouping variable in the analysis was homeless status – i.e., currently experiencing homelessness or living in a shelter – versus not experiencing homelessness.
The research team analyzed, among individuals who were and were not experiencing homelessness, whether buprenorphine compared to extended-release naltrexone was better at preventing return to use than the other, and if so, what factors accounted for that advantage.
When researchers examine factors that account for, or explain, treatment effects, they are called treatment mechanisms, or mediators. In this study, the four mediators of interest in the analysis were adherence, depressive symptoms, early illicit opioid use, and pain.
Adherence was included as a proportion for the dose of treatment that was received over the dose of treatment that should have been received. For individuals in the extended-release naltrexone group, this was calculated as the number of injections that were received divided by the number of injections that should have been received. For individuals in the buprenorphine-naloxone group, this was calculated as the number of days between the first and last dose divided by the number of days between the start (treatment initiation) and end of follow-up (date of dropout). Depressive symptoms were measured on a continuous scale where higher values indicated more symptoms. Early illicit opioid use was measured following treatment initiation and before 4 weeks after discharge or date of relapse/dropout: it was defined as any illicit opioid use versus none and could be self-reported or detected in urine testing.
Individuals with chronic pain that required the use of opioids to help manage the pain were not eligible for the trial; thus, pain was an indication of a participant’s pain or discomfort rating on the day of their assessment (measured by the EuroQOL as none, moderate or extreme). The authors also included other variables in their model to control for potential key differences between the groups (such as gender, age, and level of education).
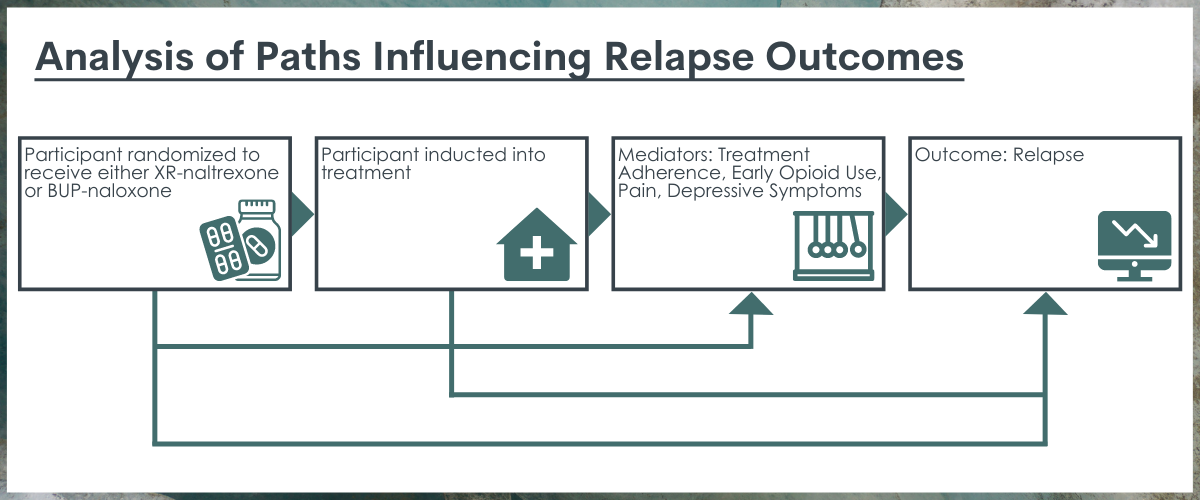
Path analysis used in the study. This framework was used by the researchers to analyze the ways in which the various parts of the path, including the 4 relevant mediators, interact to influence relapse outcomes.
This sample of 570 individuals with opioid use disorder who presented for inpatient treatment were primarily not experiencing homelessness (75%). Overall, the study sample was 34 years old, on average, 70% male, 75% White and 10% Black and 13-20% Latino. Most participants used heroin (80%), more than 60% reported injecting drugs, and 35-40% had prior treatment. Participants commonly reported using other substances in the past 30 days: 47-57% with stimulant use, 25-32% with sedative use, 42-48% with cannabis use, and 25-27% with “heavy” drinking levels. Individuals were not allowed to participate in the study if they had “serious medical, psychiatric, or substance use disorder” as determined by the study physician, but nearly 70% did report a lifetime history of some type of psychiatric disorder and overall, the sample had on average “mild” depressive symptoms as measured by the Hamilton Depression Scale.
WHAT DID THIS STUDY FIND?
Individuals who were experiencing homelessness responded better to extended-release naltrexone while non-homeless individuals responded better to buprenorphine.
Across both groups, there was a lower likelihood of treatment initiation when assigned to the extended-release naltrexone group, but the effect size for people experiencing homelessness was approximately half that for individuals who were not experiencing homelessness. This finding indicates that people experiencing homelessness were more likely than those not experiencing homelessness to initiate extended-release naltrexone. As well, individuals experiencing homelessness were 16% less likely to return to opioid use on extended-release naltrexone versus buprenorphine–naloxone while individuals not experiencing homelessness were 16% more likely to return to opioid use on extended-release naltrexone.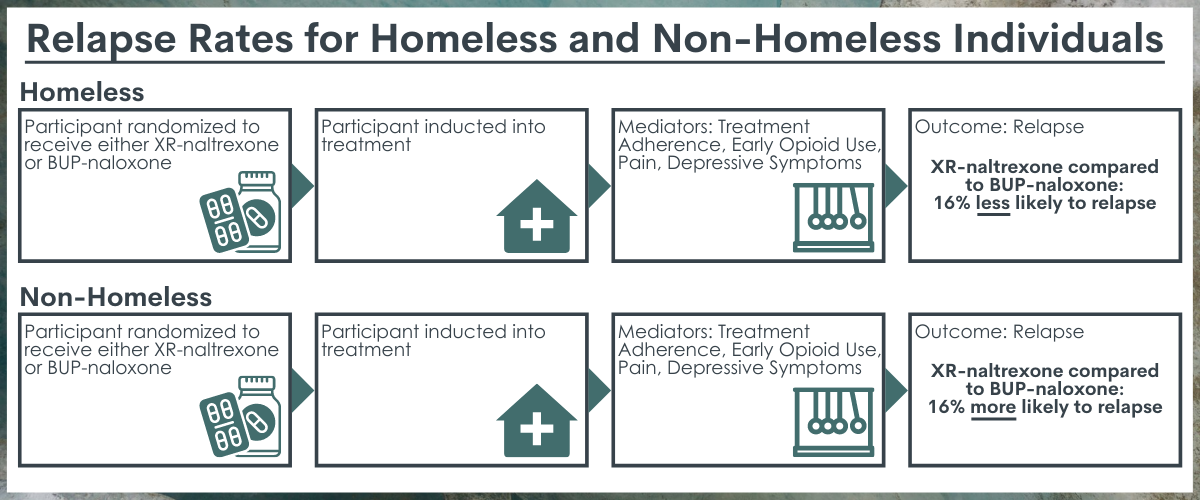
Treatment assignment influenced early illicit opioid use and depressive symptoms among individuals not experiencing homelessness.
For individuals who were not experiencing homelessness, assignment to the extended-release naltrexone versus the buprenorphine-naloxone treatment predicted early illicit opioid use and increased depressive symptoms. Yet, these treatment assignment differences did not apply to individuals experiencing homelessness: there were no differences in early illicit opioid use or depressive outcomes between the extended-release naltrexone and the buprenorphine-naloxone treatment groups. Furthermore, there were no differences in pain outcomes between the treatment groups by their status of experiencing homelessness or not.
Adherence, early illicit opioid use, depressive symptoms and pain were important to the relationship between treatment assignment, initiation, and relapse but only for individuals who were not homeless.
Adherence, early illicit opioid use, depressive symptoms and pain together explained a fifth of the relationship between medication assignment/initiation and risk of return to opioid use on extended-release naltrexone versus buprenorphine–naloxone for individuals who were not experiencing homelessness. The same factors did not substantially contribute to the risk of return to opioid use among people experiencing homelessness. Importantly, though, for both homeless and non-homeless individuals, none of the tested mediators predicted relapse. That is, neither medication adherence, depressive symptoms, pain, nor early opioid use predicted whether or not participants relapsed for either of the groups.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
The researchers of the original study from which the current study was conducted explored predictors of sustained engagement in medication treatment for opioid use disorder among individuals participating in a large randomized controlled trial that involved assignment to either extended-release naltrexone or buprenorphine-naloxone. In this secondary data analysis, they found that there were different initiation, adherence, and treatment outcomes between individuals experiencing homelessness versus those who were not experiencing homelessness.
Notably, individuals who were experiencing homelessness were more likely than those not experiencing homelessness to actually initiate treatment, when the assigned treatment was the extended-release naltrexone. They were also less likely to return to opioid use when assigned to the extended-release naltrexone group.
Homeless individuals experience many challenges that would make it hard to establish the abstinence needed to initiate extended-release naltrexone. In this study, though, participants were recruited from inpatient detoxification programs, which help to support this initial period of complete abstinence. It is unclear why homeless individuals responded better to extended-release naltrexone not only over time but immediately upon initiation. If, in fact, the monthly dosing was more motivating for homeless individuals, future work might investigate whether periodic buprenorphine injections produces similar or better outcomes than extended-release naltrexone injections. Yet, overall, there was a lower likelihood of treatment initiation among individuals assigned to the extended-release naltrexone group, indicating that despite this relative success, there are still barriers to successfully implementing this form of treatment which requires an initial period of abstinence to start.
Additionally, the research team was able to identify several factors that as a bundle together may help to explain the pathway from treatment initiation and the risk of return to opioid use among individuals who were not experiencing homelessness: these factors include adherence, early illicit opioid use, depressive symptoms, and pain.
The findings raise several future research directions. First, especially given the absence of association between reduced depressive symptoms and opioid outcomes, more research on how depressive symptoms change as a function of treatment and what implications this has for individual recoveries should be addressed. For example, other research has suggested that both buprenorphine and extended-release naltrexone can be successful in reducing depression symptoms while reducing risk of return to use. At the same time, research also indicates a history of major depressive disorder may result in better opioid use outcomes for individuals prescribed buprenorphine. Although this may be a counterintuitive finding, it is possible that such individuals may have developed coping skills through their experience overcoming mental health challenges, skills that also assist their recovery process.
Yet, these factors were related to the benefit of buprenorphine for individuals who were not experiencing homelessness, they did not help to explain the corresponding benefit of extended-release naltrexone for individuals experiencing homelessness. Thus, there is a need to better understand what factors contribute to the medication treatment experience of individuals experiencing homelessness so that practitioners and systems can specifically target any barriers to treatment initiation and adherence.
- LIMITATIONS
-
- This study did not have a reliable measure of the actual doses of buprenorphine-naloxone taken each day as the research team only captured the number of doses provided to patients. Thus, the adherence calculation assumes perfect adherence, and does not address instances where medication was lost, sold, or simply avoided (discarded).
- In this comparison of buprenorphine-naloxone and extended-release naltrexone, there is an inherent confounding between the mode of medication delivery (injection versus pill) and timeline of delivery (daily versus monthly). As a result, we cannot link adherence or outcomes directly to the medication differences; as research that examines injectable buprenorphine outcomes suggests this is a viable alternative to the daily pill, future research should examine this modality along with key participant characteristics.
- Despite the use of random assignment to treatment condition in this study, it is possible there were additional confounders not addressed in their analysis model, a model which assumes there are no unobserved and important variables; this limitation seems likely as there were some differences between those experiencing homelessness and those not. If there were key missing variables in the models, then some of the relationships could be artificially inflated.
- Whether or not the patients were engaged in additional other evidence-based psychosocial treatments and supports, such as meditation/mindfulness, self-help groups, or targeted mental health services for comorbid conditions such as depression were not measured; thus, it is possible that some patients saw improvements in various aspects of their lives due to treatments outside the medication, which enabled them to sustain their recovery process and adhere to the medication regimen.
BOTTOM LINE
The researchers found that among a population of individuals seeking inpatient detoxification for opioid use disorders, individuals were more likely to initiate buprenorphine-naloxone compared to extended-release naltrexone medication treatment. Yet, individuals experiencing homelessness were more likely than those not experiencing homelessness to initiate extended-release naltrexone and had better outcomes than those assigned to receive buprenorphine, suggesting this monthly opioid antagonist injection might be preferred to daily buprenorphine among this population. Although several factors together seemed important to the recovery process among individuals who were not experiencing homelessness (adherence to their assigned medication, early illicit use of opioids, depressive symptoms, and pain), there remains a gap in our understanding of key mediators of the process of treatment initiation and outcomes among individuals with an opioid use disorder. This gap is especially noticeable for individuals with unique needs, such as those experiencing homelessness.
- For individuals and families seeking recovery: If you or your loved one has an opioid use disorder, both of the medications used in this study could help reduce craving and protect against a return to opioid use. Extended-release naltrexone may be harder to start as it requires a period of at least a few days of opioid abstinence, but may also be easier to continue once started, and for some, may increase the likelihood of maintaining abstinence in the long-term. If you are starting on either medication, it is important to discuss with your provider what barriers you may encounter and have a plan about how to best find support to address them.
- For treatment professionals and treatment systems: Despite the benefits of medication treatment for opioid use disorder, there are many barriers to initiating and maintaining these treatments and these factors vary by the individual patient. In general, working with patients directly to address their unique barriers may help sustain their recovery experience. For example, individuals experiencing homelessness may have different motivations for initiating treatments that do not add further burden to their existing suite of challenges; thus, they may require different supports than individuals who are not experiencing homelessness to initiate and sustain treatment adherence over time.
- For scientists: Despite the identification of a bundle of key factors among individuals who were not experiencing homelessness, there is a need to address how these factors work in recovery pathways and how they may be targeted in future intervention and treatment research. Additionally, although there were some positive outcomes for individuals experiencing homelessness, the findings do not point to specific mediators of treatment success for this population; future research to understand why the monthly injection extended-release naltrexone produced better outcomes than daily buprenorphine may help improve outcomes for this vulnerable group.
- For policy makers: As others have suggested, there may be a need to revamp our system of care to better support the detoxification and treatment initiation process to improve patient outcomes; a similar study in Norway where there is more public health support for longer inpatient treatment stays found no differences in treatment initiation between buprenorphine and extended-release naltrexone groups, a finding that suggests that more support during this crucial phase could greatly increase long-term treatment success.
CITATIONS
Rudolph, K. E., Díaz, I., Hejazi, N. S., van der Laan, M. J., Luo, S. X., Shulman, M., . . . & Nunes, E. V. (2021). Explaining differential effects of medication for opioid use disorder using a novel approach incorporating mediating variables. Addiction, 116(8), 2094-2103. doi: 10.1111/add.15377

