l
A major contributor to the ongoing drug overdose crisis in Canada, Europe, and the US is reliance on an unregulated drug supply that may be contaminated with toxic substances, such as fentanyl. This led to a recent call by British Columbia’s chief coroner to reduce people’s dependence on the unregulated drug supply by offering people who use drugs an alternative. As a result, several safer supply programs are beginning to be implemented, although they remain controversial. These programs provide substances with known doses and compositions to people who use drugs, often through prescriptions, thereby decreasing their use of drugs from an unregulated supply. The limited research that has been done to evaluate safer supply programs has shown several benefits, such as increased access to healthcare and reduced use of unregulated opioids, though not in all cases.
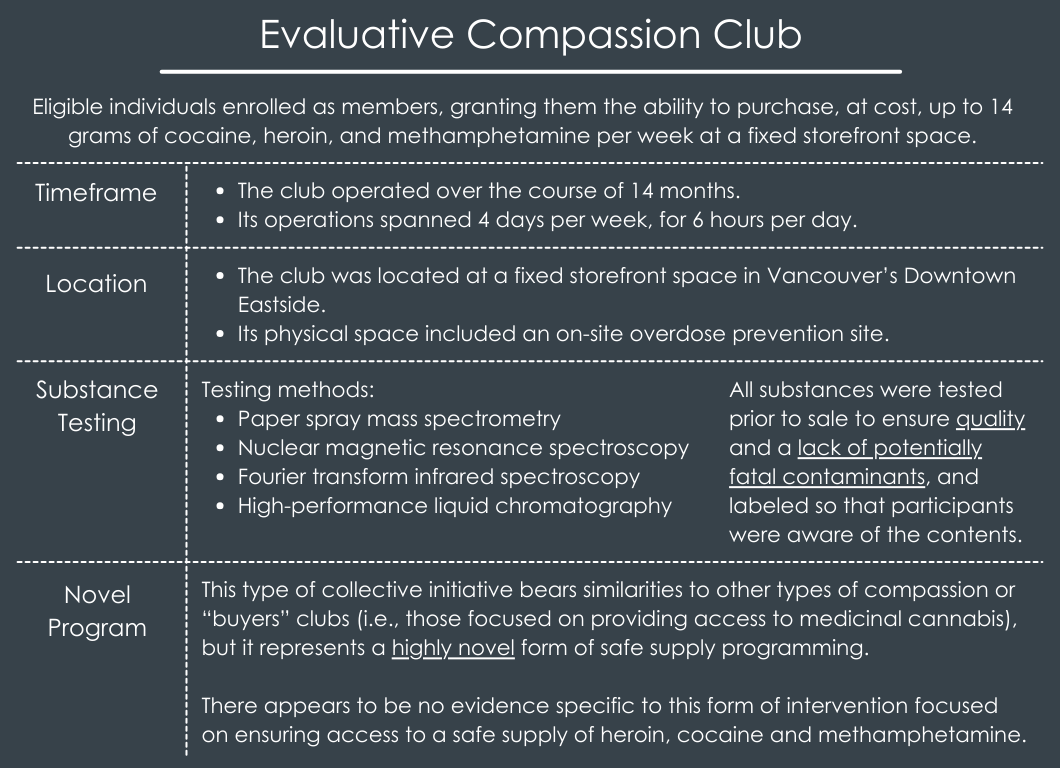
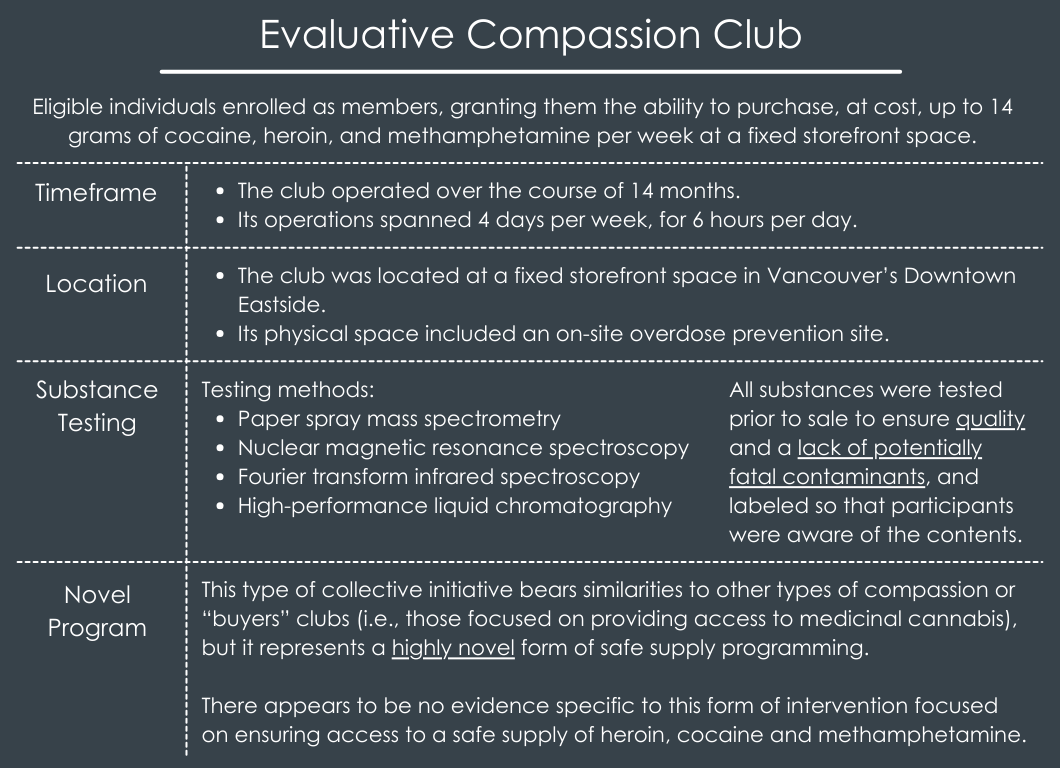
Only medicalized programs that provide drugs through prescriptions have been scaled-up in Canada, since non-medicalized programs are not sanctioned. Non-medicalized programs include “compassion clubs”, where substances of known compositions are distributed to its members. Although they failed to obtain a federal exemption to operate, the Drug Users Liberation Front piloted a Compassion Club for people who use cocaine, heroin, or methamphetamine in August 2022. This club serves people who live in Vancouver’s Downtown Eastside and are at high risk of overdose. Members can purchase up to 14 grams of cocaine, heroin, and methamphetamine per week at a storefront. Substances are tested to ensure they are safe and not contaminated.
Compassion clubs such as this are a very new approach to provide a safer supply of drugs and little is known about their public health impact. Researchers in this study examined the association between club membership and impact on non-fatal overdoses. Such research can shed light on the public health impact of non-medicalized safer supply programs.
The research team surveyed 47 compassion club members to assess whether time periods they were enrolled in the club – determined by lottery from 5 organized groups of people who use drugs in Vancouver –were associated with reduced odds of overdose relative to time periods they were not enrolled in the club over 14 months. Participants were over the age of 19, currently using drugs, and assessed as being at risk of overdose, defined as all people using drugs in the club setting, given the local drug supply’s contamination and the overall high incidence of overdose deaths.
Surveys were conducted in a private office at the compassion club that was opened by Drug Users Liberation Front in 2022. Survey data were collected by a trained research assistant every 3 months and included 3 yes or no questions assessing whether: (1) they ever had an overdose; (2) they had an overdose during the last 3 months (or since their last survey); and (3) they had an overdose where naloxone was administered during the last 3 months (or since their last survey). They were also asked if they had shared any of the drugs they obtained from the club and if so, why. Prior to enrolling in the club, participants completed 1-2 surveys. After enrolling in the club, participants completed a maximum of 5 surveys.
The primary outcomes of interest were any non-fatal overdose, which included overdose from any drug, and any non-fatal overdose where naloxone was administered, which was more specific to opioid-related overdoses (given that naloxone is used to reverse opioid-related overdoses). The primary predictor was enrollment in the Compassion Club in the last 3 months. The research team was also interested in whether the following variables could confound the possible relationship between club membership and overdoses: age at baseline, ethnicity, sex, unstable housing in the last 3 months (treated as a variable with 2 categories, one consisting of being homeless, living in a shelter or hotel, and staying with friends or family and the other defined as living in a house/apartment), and previous number of overdoses experienced throughout participants’ lives (treated as a variable with 2 categories consisting of more than 3 overdoses or less than 3).
A total of 47 people participated in the study. Initially 21 individuals were admitted to the club and then another 28 were admitted when capacity increased, but 2 of these people withdrew from the study. Of these, the median age was 47 years old and 18 identified as women. Regarding ethnicity, 29 identified as White, 23 identified as Indigenous, and 4 identified as being of other ethnicities. Approximately half of participants (23) reported experiencing unstable housing in the last 3 months. The majority of participants reported having had a non-fatal overdose throughout their life (36) and many reported having had an overdose in the 3 months before their baseline survey (34). During the study period, 22 participants reported experiencing at least one non-fatal overdose of any type and 18 reported experiencing at least one non-fatal overdose involving naloxone (i.e., was opioid-related).
Compassion club enrollment associated with reduced likelihood of non-fatal overdose of any kind
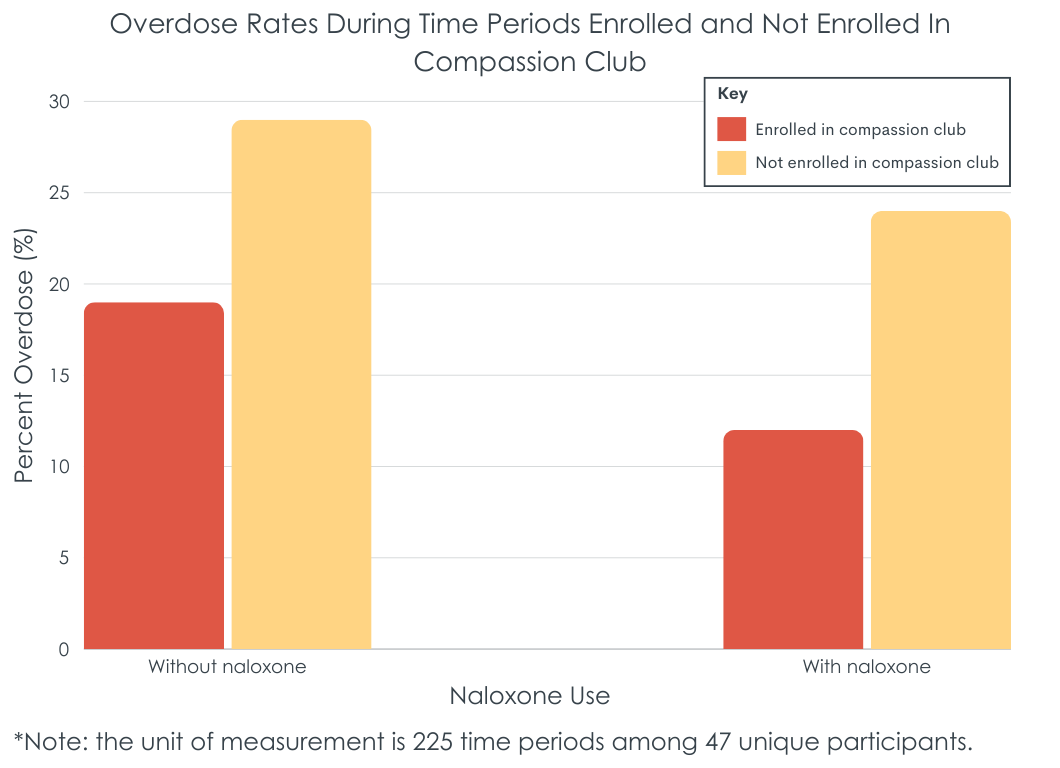
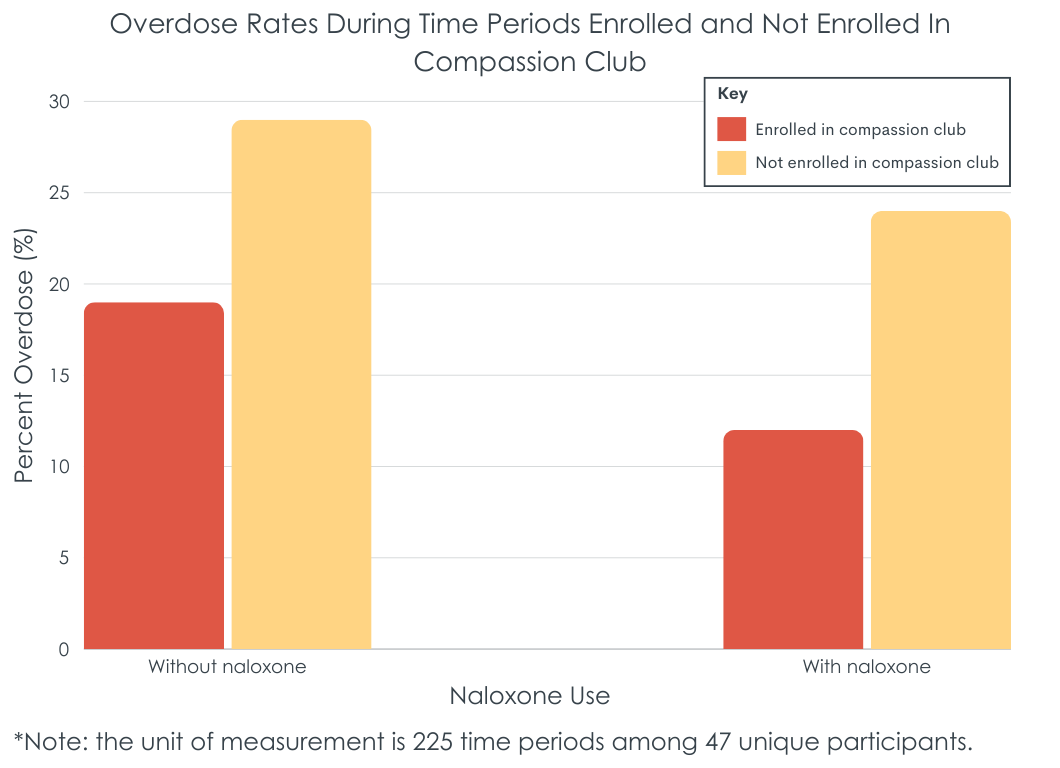
Compassion club membership reduced the likelihood of non-fatal overdose of any kind by about half (see figure below). There was also an association between sex and overdose history – women and those who identified as non-binary having a 78% lower likelihood of non-fatal overdose of any kind than men. Those who had 3 or more overdoses throughout their lives had about a 4-fold increase in the likelihood of this kind of overdose as compared to those who had fewer than 3 overdoses throughout their lives.
Compassion club enrollment associated with reduced likelihood of non-fatal overdose involving naloxone
Compassion club membership reduced the likelihood of non-fatal overdose involving naloxone by 63% (see figure below). Women and those who identified as non-binary had an 89% lower likelihood of non-fatal overdose of any kind than men; those who identified as White had a 70% lower likelihood than those of other ethnicities. Those who had 3 or more overdoses throughout their lives had about a 5-fold increase in the likelihood of this kind of overdose as compared to those who had fewer than 3 overdoses throughout their lives.
Times when participants were enrolled in an unsanctioned “compassion club” that provides access to a tested safer supply of cocaine, heroin, or methamphetamine, were associated with reduced overdose risk compared to times they were not enrolled in the club. It is possible that individuals were enrolled in the club during times they were more motivated to use their drug of choice in safer ways, overall. That said, the study controlled statistically for factors that could influence the association between enrollment and overdose, such as unstable housing (e.g., with drug use in more precarious settings and situations). Given the clear conceptual link between safer supply with rigorously tested drugs and lower overdose, it is plausible, if not likely, that club enrollment was causally related to the reduced overdose rates observed in the study.
Additionally, the finding that the chance of any kind, as well as opioid-specific, overdose was lower for women and those identifying as non-binary (compared with men) could be related to their typically lower levels of impulsivity. Likewise, White ethnicity being associated with a lower likelihood of opioid-related overdoses than other ethnicities is consistent with recent trends showing a shift in the opioid crisis from a larger impact on White people to a larger impact on Black people. Finally, the finding that the likelihood of any, as well as opioid-specific, overdoses was lower for people who experienced fewer overdoses throughout their lives is not that surprising, given that people who have experienced more overdoses typically have more chronic courses of addiction and may have a more severe form of substance use disorder.
This study’s key finding – that membership in an unsanctioned, non-medicalized safer supply program was associated with a lower chance of any and opioid-related overdoses – add to the to the growing number of harm reduction strategies suggesting public health benefits. Importantly however, non-medicalized safer supply programs such as the compassion club in this study, as well as the large majority of harm reduction approaches, remain either illegal or without formal policy support to legally operate. This limits the extent to which researchers can analyze in a more rigorous scientific manner their impact on overdoses and public health. Accordingly, policy changes are needed, given the continuing overdose crisis and potential of safer supply programs to save lives and improve public health.
Enrollment in a compassion club, which provides members with rigorously tested, and therefore safer drugs, was associated with reduced likelihood of experiencing a non-fatal overdose from any drug and from opioids. The likelihood of any and opioid-related overdoses was also lower for women and for those who have experienced fewer than 3 overdoses throughout their lives.
Kalicum, J., Nyx, E., Kennedy, M. C., & Kerr, T. (2024). The impact of an unsanctioned compassion club on non-fatal overdose. International Journal of Drug Policy, 131. doi: 10.1016/j.drugpo.2024.104330.
l
A major contributor to the ongoing drug overdose crisis in Canada, Europe, and the US is reliance on an unregulated drug supply that may be contaminated with toxic substances, such as fentanyl. This led to a recent call by British Columbia’s chief coroner to reduce people’s dependence on the unregulated drug supply by offering people who use drugs an alternative. As a result, several safer supply programs are beginning to be implemented, although they remain controversial. These programs provide substances with known doses and compositions to people who use drugs, often through prescriptions, thereby decreasing their use of drugs from an unregulated supply. The limited research that has been done to evaluate safer supply programs has shown several benefits, such as increased access to healthcare and reduced use of unregulated opioids, though not in all cases.
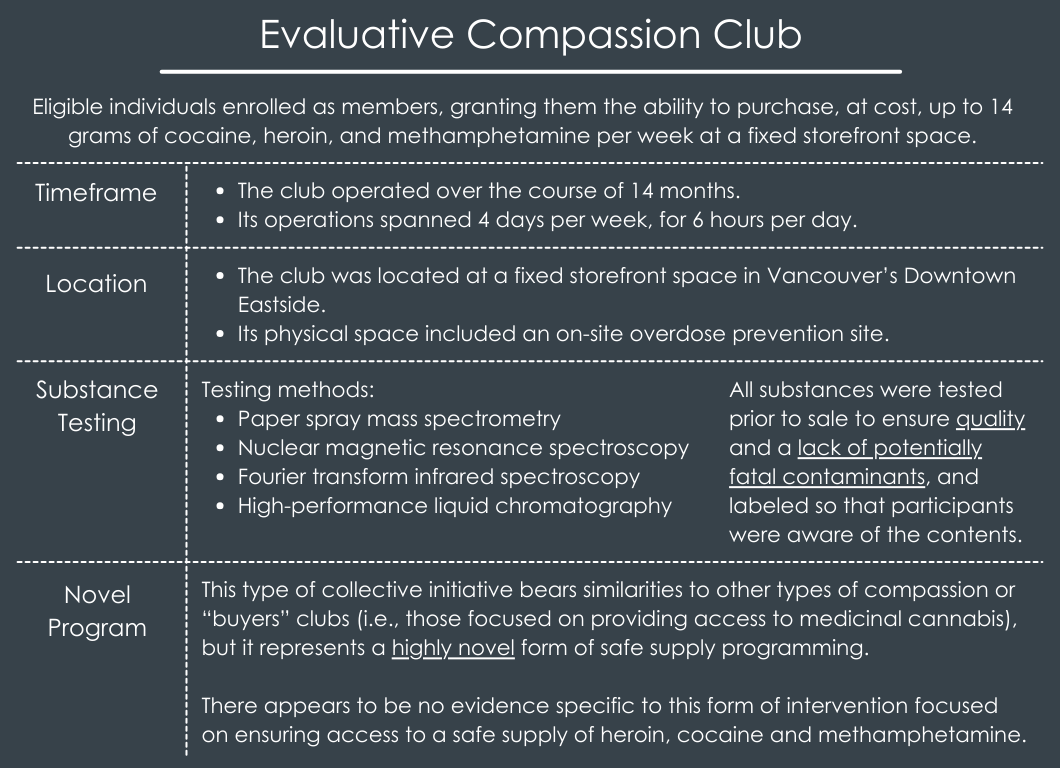
Only medicalized programs that provide drugs through prescriptions have been scaled-up in Canada, since non-medicalized programs are not sanctioned. Non-medicalized programs include “compassion clubs”, where substances of known compositions are distributed to its members. Although they failed to obtain a federal exemption to operate, the Drug Users Liberation Front piloted a Compassion Club for people who use cocaine, heroin, or methamphetamine in August 2022. This club serves people who live in Vancouver’s Downtown Eastside and are at high risk of overdose. Members can purchase up to 14 grams of cocaine, heroin, and methamphetamine per week at a storefront. Substances are tested to ensure they are safe and not contaminated.
Compassion clubs such as this are a very new approach to provide a safer supply of drugs and little is known about their public health impact. Researchers in this study examined the association between club membership and impact on non-fatal overdoses. Such research can shed light on the public health impact of non-medicalized safer supply programs.
The research team surveyed 47 compassion club members to assess whether time periods they were enrolled in the club – determined by lottery from 5 organized groups of people who use drugs in Vancouver –were associated with reduced odds of overdose relative to time periods they were not enrolled in the club over 14 months. Participants were over the age of 19, currently using drugs, and assessed as being at risk of overdose, defined as all people using drugs in the club setting, given the local drug supply’s contamination and the overall high incidence of overdose deaths.
Surveys were conducted in a private office at the compassion club that was opened by Drug Users Liberation Front in 2022. Survey data were collected by a trained research assistant every 3 months and included 3 yes or no questions assessing whether: (1) they ever had an overdose; (2) they had an overdose during the last 3 months (or since their last survey); and (3) they had an overdose where naloxone was administered during the last 3 months (or since their last survey). They were also asked if they had shared any of the drugs they obtained from the club and if so, why. Prior to enrolling in the club, participants completed 1-2 surveys. After enrolling in the club, participants completed a maximum of 5 surveys.
The primary outcomes of interest were any non-fatal overdose, which included overdose from any drug, and any non-fatal overdose where naloxone was administered, which was more specific to opioid-related overdoses (given that naloxone is used to reverse opioid-related overdoses). The primary predictor was enrollment in the Compassion Club in the last 3 months. The research team was also interested in whether the following variables could confound the possible relationship between club membership and overdoses: age at baseline, ethnicity, sex, unstable housing in the last 3 months (treated as a variable with 2 categories, one consisting of being homeless, living in a shelter or hotel, and staying with friends or family and the other defined as living in a house/apartment), and previous number of overdoses experienced throughout participants’ lives (treated as a variable with 2 categories consisting of more than 3 overdoses or less than 3).
A total of 47 people participated in the study. Initially 21 individuals were admitted to the club and then another 28 were admitted when capacity increased, but 2 of these people withdrew from the study. Of these, the median age was 47 years old and 18 identified as women. Regarding ethnicity, 29 identified as White, 23 identified as Indigenous, and 4 identified as being of other ethnicities. Approximately half of participants (23) reported experiencing unstable housing in the last 3 months. The majority of participants reported having had a non-fatal overdose throughout their life (36) and many reported having had an overdose in the 3 months before their baseline survey (34). During the study period, 22 participants reported experiencing at least one non-fatal overdose of any type and 18 reported experiencing at least one non-fatal overdose involving naloxone (i.e., was opioid-related).
Compassion club enrollment associated with reduced likelihood of non-fatal overdose of any kind
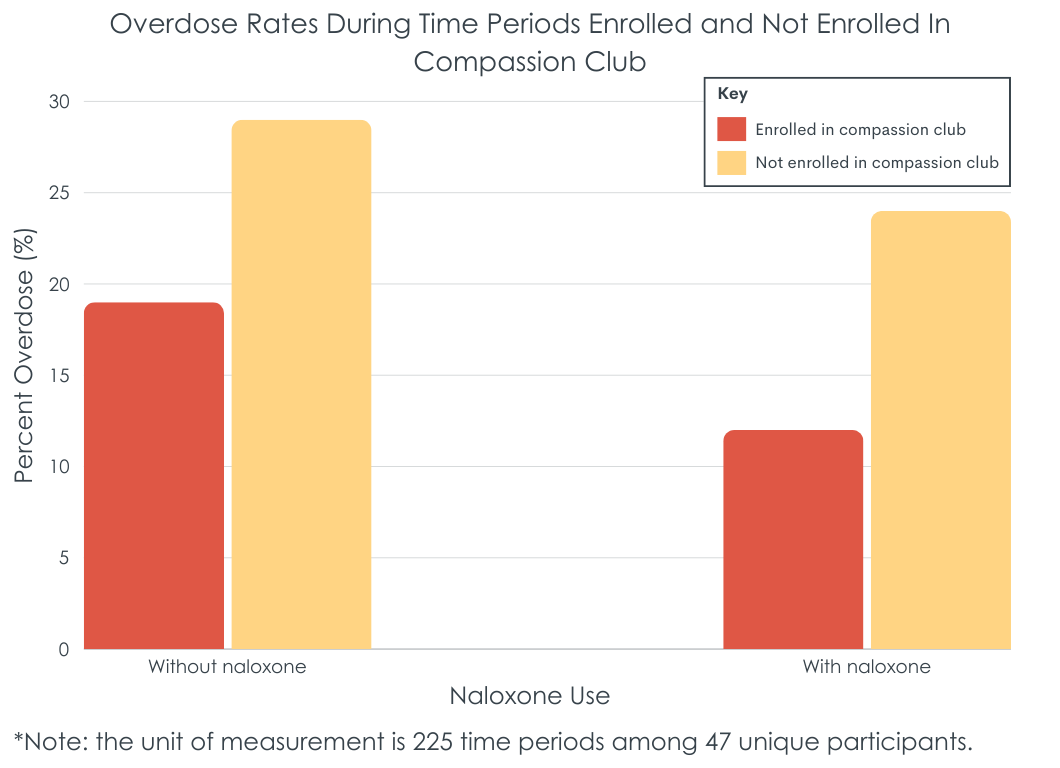
Compassion club membership reduced the likelihood of non-fatal overdose of any kind by about half (see figure below). There was also an association between sex and overdose history – women and those who identified as non-binary having a 78% lower likelihood of non-fatal overdose of any kind than men. Those who had 3 or more overdoses throughout their lives had about a 4-fold increase in the likelihood of this kind of overdose as compared to those who had fewer than 3 overdoses throughout their lives.
Compassion club enrollment associated with reduced likelihood of non-fatal overdose involving naloxone
Compassion club membership reduced the likelihood of non-fatal overdose involving naloxone by 63% (see figure below). Women and those who identified as non-binary had an 89% lower likelihood of non-fatal overdose of any kind than men; those who identified as White had a 70% lower likelihood than those of other ethnicities. Those who had 3 or more overdoses throughout their lives had about a 5-fold increase in the likelihood of this kind of overdose as compared to those who had fewer than 3 overdoses throughout their lives.
Times when participants were enrolled in an unsanctioned “compassion club” that provides access to a tested safer supply of cocaine, heroin, or methamphetamine, were associated with reduced overdose risk compared to times they were not enrolled in the club. It is possible that individuals were enrolled in the club during times they were more motivated to use their drug of choice in safer ways, overall. That said, the study controlled statistically for factors that could influence the association between enrollment and overdose, such as unstable housing (e.g., with drug use in more precarious settings and situations). Given the clear conceptual link between safer supply with rigorously tested drugs and lower overdose, it is plausible, if not likely, that club enrollment was causally related to the reduced overdose rates observed in the study.
Additionally, the finding that the chance of any kind, as well as opioid-specific, overdose was lower for women and those identifying as non-binary (compared with men) could be related to their typically lower levels of impulsivity. Likewise, White ethnicity being associated with a lower likelihood of opioid-related overdoses than other ethnicities is consistent with recent trends showing a shift in the opioid crisis from a larger impact on White people to a larger impact on Black people. Finally, the finding that the likelihood of any, as well as opioid-specific, overdoses was lower for people who experienced fewer overdoses throughout their lives is not that surprising, given that people who have experienced more overdoses typically have more chronic courses of addiction and may have a more severe form of substance use disorder.
This study’s key finding – that membership in an unsanctioned, non-medicalized safer supply program was associated with a lower chance of any and opioid-related overdoses – add to the to the growing number of harm reduction strategies suggesting public health benefits. Importantly however, non-medicalized safer supply programs such as the compassion club in this study, as well as the large majority of harm reduction approaches, remain either illegal or without formal policy support to legally operate. This limits the extent to which researchers can analyze in a more rigorous scientific manner their impact on overdoses and public health. Accordingly, policy changes are needed, given the continuing overdose crisis and potential of safer supply programs to save lives and improve public health.
Enrollment in a compassion club, which provides members with rigorously tested, and therefore safer drugs, was associated with reduced likelihood of experiencing a non-fatal overdose from any drug and from opioids. The likelihood of any and opioid-related overdoses was also lower for women and for those who have experienced fewer than 3 overdoses throughout their lives.
Kalicum, J., Nyx, E., Kennedy, M. C., & Kerr, T. (2024). The impact of an unsanctioned compassion club on non-fatal overdose. International Journal of Drug Policy, 131. doi: 10.1016/j.drugpo.2024.104330.
l
A major contributor to the ongoing drug overdose crisis in Canada, Europe, and the US is reliance on an unregulated drug supply that may be contaminated with toxic substances, such as fentanyl. This led to a recent call by British Columbia’s chief coroner to reduce people’s dependence on the unregulated drug supply by offering people who use drugs an alternative. As a result, several safer supply programs are beginning to be implemented, although they remain controversial. These programs provide substances with known doses and compositions to people who use drugs, often through prescriptions, thereby decreasing their use of drugs from an unregulated supply. The limited research that has been done to evaluate safer supply programs has shown several benefits, such as increased access to healthcare and reduced use of unregulated opioids, though not in all cases.
Only medicalized programs that provide drugs through prescriptions have been scaled-up in Canada, since non-medicalized programs are not sanctioned. Non-medicalized programs include “compassion clubs”, where substances of known compositions are distributed to its members. Although they failed to obtain a federal exemption to operate, the Drug Users Liberation Front piloted a Compassion Club for people who use cocaine, heroin, or methamphetamine in August 2022. This club serves people who live in Vancouver’s Downtown Eastside and are at high risk of overdose. Members can purchase up to 14 grams of cocaine, heroin, and methamphetamine per week at a storefront. Substances are tested to ensure they are safe and not contaminated.
Compassion clubs such as this are a very new approach to provide a safer supply of drugs and little is known about their public health impact. Researchers in this study examined the association between club membership and impact on non-fatal overdoses. Such research can shed light on the public health impact of non-medicalized safer supply programs.
The research team surveyed 47 compassion club members to assess whether time periods they were enrolled in the club – determined by lottery from 5 organized groups of people who use drugs in Vancouver –were associated with reduced odds of overdose relative to time periods they were not enrolled in the club over 14 months. Participants were over the age of 19, currently using drugs, and assessed as being at risk of overdose, defined as all people using drugs in the club setting, given the local drug supply’s contamination and the overall high incidence of overdose deaths.
Surveys were conducted in a private office at the compassion club that was opened by Drug Users Liberation Front in 2022. Survey data were collected by a trained research assistant every 3 months and included 3 yes or no questions assessing whether: (1) they ever had an overdose; (2) they had an overdose during the last 3 months (or since their last survey); and (3) they had an overdose where naloxone was administered during the last 3 months (or since their last survey). They were also asked if they had shared any of the drugs they obtained from the club and if so, why. Prior to enrolling in the club, participants completed 1-2 surveys. After enrolling in the club, participants completed a maximum of 5 surveys.
The primary outcomes of interest were any non-fatal overdose, which included overdose from any drug, and any non-fatal overdose where naloxone was administered, which was more specific to opioid-related overdoses (given that naloxone is used to reverse opioid-related overdoses). The primary predictor was enrollment in the Compassion Club in the last 3 months. The research team was also interested in whether the following variables could confound the possible relationship between club membership and overdoses: age at baseline, ethnicity, sex, unstable housing in the last 3 months (treated as a variable with 2 categories, one consisting of being homeless, living in a shelter or hotel, and staying with friends or family and the other defined as living in a house/apartment), and previous number of overdoses experienced throughout participants’ lives (treated as a variable with 2 categories consisting of more than 3 overdoses or less than 3).
A total of 47 people participated in the study. Initially 21 individuals were admitted to the club and then another 28 were admitted when capacity increased, but 2 of these people withdrew from the study. Of these, the median age was 47 years old and 18 identified as women. Regarding ethnicity, 29 identified as White, 23 identified as Indigenous, and 4 identified as being of other ethnicities. Approximately half of participants (23) reported experiencing unstable housing in the last 3 months. The majority of participants reported having had a non-fatal overdose throughout their life (36) and many reported having had an overdose in the 3 months before their baseline survey (34). During the study period, 22 participants reported experiencing at least one non-fatal overdose of any type and 18 reported experiencing at least one non-fatal overdose involving naloxone (i.e., was opioid-related).
Compassion club enrollment associated with reduced likelihood of non-fatal overdose of any kind
Compassion club membership reduced the likelihood of non-fatal overdose of any kind by about half (see figure below). There was also an association between sex and overdose history – women and those who identified as non-binary having a 78% lower likelihood of non-fatal overdose of any kind than men. Those who had 3 or more overdoses throughout their lives had about a 4-fold increase in the likelihood of this kind of overdose as compared to those who had fewer than 3 overdoses throughout their lives.
Compassion club enrollment associated with reduced likelihood of non-fatal overdose involving naloxone
Compassion club membership reduced the likelihood of non-fatal overdose involving naloxone by 63% (see figure below). Women and those who identified as non-binary had an 89% lower likelihood of non-fatal overdose of any kind than men; those who identified as White had a 70% lower likelihood than those of other ethnicities. Those who had 3 or more overdoses throughout their lives had about a 5-fold increase in the likelihood of this kind of overdose as compared to those who had fewer than 3 overdoses throughout their lives.
Times when participants were enrolled in an unsanctioned “compassion club” that provides access to a tested safer supply of cocaine, heroin, or methamphetamine, were associated with reduced overdose risk compared to times they were not enrolled in the club. It is possible that individuals were enrolled in the club during times they were more motivated to use their drug of choice in safer ways, overall. That said, the study controlled statistically for factors that could influence the association between enrollment and overdose, such as unstable housing (e.g., with drug use in more precarious settings and situations). Given the clear conceptual link between safer supply with rigorously tested drugs and lower overdose, it is plausible, if not likely, that club enrollment was causally related to the reduced overdose rates observed in the study.
Additionally, the finding that the chance of any kind, as well as opioid-specific, overdose was lower for women and those identifying as non-binary (compared with men) could be related to their typically lower levels of impulsivity. Likewise, White ethnicity being associated with a lower likelihood of opioid-related overdoses than other ethnicities is consistent with recent trends showing a shift in the opioid crisis from a larger impact on White people to a larger impact on Black people. Finally, the finding that the likelihood of any, as well as opioid-specific, overdoses was lower for people who experienced fewer overdoses throughout their lives is not that surprising, given that people who have experienced more overdoses typically have more chronic courses of addiction and may have a more severe form of substance use disorder.
This study’s key finding – that membership in an unsanctioned, non-medicalized safer supply program was associated with a lower chance of any and opioid-related overdoses – add to the to the growing number of harm reduction strategies suggesting public health benefits. Importantly however, non-medicalized safer supply programs such as the compassion club in this study, as well as the large majority of harm reduction approaches, remain either illegal or without formal policy support to legally operate. This limits the extent to which researchers can analyze in a more rigorous scientific manner their impact on overdoses and public health. Accordingly, policy changes are needed, given the continuing overdose crisis and potential of safer supply programs to save lives and improve public health.
Enrollment in a compassion club, which provides members with rigorously tested, and therefore safer drugs, was associated with reduced likelihood of experiencing a non-fatal overdose from any drug and from opioids. The likelihood of any and opioid-related overdoses was also lower for women and for those who have experienced fewer than 3 overdoses throughout their lives.
Kalicum, J., Nyx, E., Kennedy, M. C., & Kerr, T. (2024). The impact of an unsanctioned compassion club on non-fatal overdose. International Journal of Drug Policy, 131. doi: 10.1016/j.drugpo.2024.104330.
151 Merrimac St., 4th Floor. Boston, MA 02114