Does where you live affect your genetic risk of developing problematic alcohol use?
There is scientific consensus that genetics influence whether drinking will ultimately lead to alcohol use disorder and other harmful forms of drinking. What happens when those who are genetically predisposed to harmful drinking have less access to alcohol? In this study, authors showed that neighborhood alcohol outlet density matters. Living in neighborhoods with less access to alcohol reduces the influence of genetics on harmful drinking.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
For decades, scientists have understood that genetics factors influence who develops alcohol use disorders (AUDs). However, recent advanced genetic analyses have shown that only 9% of the variance in AUDs is explained by genes, leading scientists to hypothesize a large role for environmental factors and gene-environment interactions. The availability and accessibility of alcohol is one big environmental factor that influences rates of alcohol consumption. In this study, authors sought to answer the question of whether – and to what extent – living in a neighborhood with more alcohol outlets (bars, liquor stores) would increase the chances of someone with genetic risk for AUD developing an AUD. Data have previously shown that adolescents growing up in neighborhoods with more liquor stores were more likely to drink, and this study incorporated genetic analyses to see how this measure affected the prevalence of alcohol use disorders.
HOW WAS THIS STUDY CONDUCTED?
Participants were drawn from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a study of 15,197 adolescents in grades 7–12 in the United States during the 1994–95 school year. The Add Health cohort has been followed into young adulthood with 4 in-home interviews, the most recent in 2008, when the sample was aged 24–32. The sample included a combination of genetically identical twins, non-identical (dizygotic) twins, full biological sibling pairs, and half-biological sibling pairs. Using these groups helps researchers to understand genetic contributions to alcohol use disorders, and allows researchers to parse out effects of genetics, shared environment, and unique environment. Authors defined “alcohol problems” as the sum of 8 alcohol problems where each problem needed to occur at least once in the past year to count toward the total (i.e., maximum alcohol problem score of 8): 1) had a problem at work or school, 2) had a problem with friends, 3) had a problem with a romantic partner, 4) had a hangover, 5) became nauseous or vomited, 6) got into a sexual situation they later regretted, 7) got into a physical fight because of drinking, and 8) got drunk at school or work.
Alcohol outlet licensing data were gathered from individual states between September 2006 and June 2007. Data were obtained from 43 states and the District of Columbia; 34 of these provided both on-premises outlet (alcohol sold to be consumed on site, including bars and restaurants) and off-premises outlet (alcohol sold to be consumed elsewhere, such as liquor, convenience and grocery stores) data, and outlet licensing data. The total number of on- and off-premises outlets were divided by the total land area in order to derive the density of alcohol outlets. Authors controlled statistically for household income, state, urbanicity/population density, and neighborhood socio-demographic characteristics to try and isolate the independent effects of genetics and alcohol outlet density on alcohol problems.
WHAT DID THIS STUDY FIND?
This study found a dramatic influence of alcohol outlet density on likelihood of developing alcohol problems. In other words, if someone lived in a small town with 20 bars, this was more problematic than if someone lived in a large town with 20 bars. The genetic influence of alcohol problems for those residing in a neighborhood with more than 10 on-premises outlets was 78%, compared with 11% for those in a neighborhood with no on-premises outlets. The amplified effect on genetic risk for alcohol outlet density in increasing alcohol problems was not explained by state of residence, population density or neighborhood socio-demographic characteristics.
Outlet density did not correlate with the average amount of reported alcohol problems, indicating an interaction between genetic liability and alcohol outlet density was necessary for greater alcohol problems to occur. The implication of this finding is a “gene x environment” interaction: people without a genetic liability are much less at risk of developing AUD if they live around alcohol outlets than people with a genetic liability, who are at much greater risk.
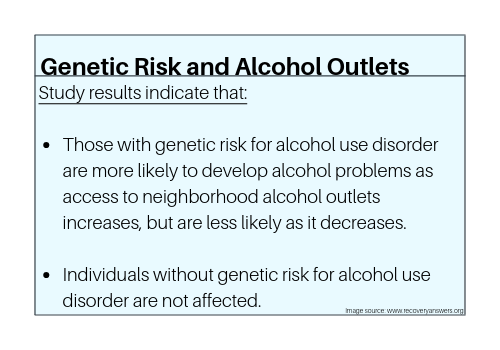
Figure 1.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
There is a variety of evidence of geographic differences in rates of alcohol use disorder, suggesting that environmental factors and gene–environment interactions are likely to play an important role in risk for AUD. This study found that in a national sample of young adults in the United States, genetic influence on risk for alcohol problems was moderated by neighborhood alcohol outlet density. In environments in which alcohol was less available, the genetic predisposition to develop problems was muted, whereas in environments in which alcohol was more readily available, the latent genetic vulnerability was amplified. This study could have policy implications, as it suggests that policies limiting alcohol outlet densities could play an important role in the prevention of alcohol problems.
Said another way, individuals at higher genetic risk for alcohol problems were more sensitive than those at lower genetic risk to the effects of living in an ‘alcogenic’ environment in which there was easy access to alcohol. This is interesting because young adults are the most common demographic group to change living locations, and it is unknown how such moves – from neighborhoods with greater to lesser alcohol outlet densities, or vice versa – impact likelihood of developing alcohol use disorders.
- LIMITATIONS
-
- The best way to conduct this study would be to only examine twins; however, the modest sample size made it necessary to include data from full and half-siblings (for whom the model assumption of perfectly correlated shared environments may not apply).
- Although there may be important sex differences in how genetic and environmental influences on alcohol involvement are moderated by neighborhood environmental characteristics, this study combined data from men and women in the analyses. Similarly, although the sample was racially diverse, the study combined data from individuals from different racial/ethnic groups. Thus, whether these findings apply equally to women vs. men and racial/ethnic minorities compared to White individuals is unclear.
- Although the assessment of alcohol problems was conducted in 2001–02, the densities of alcohol outlets were based on licensing data acquired 5 years later, in 2006– 07. The indices of the current neighborhood alcohol outlet densities may have been under or overestimated.
- Another limitation was the use of a single measure of alcohol outlet density; that is, the number of outlets per square kilometer. Future studies could examine clusters of outlets, which could lead to social aggregation of excessive drinkers in a limited geographic area, and potentially increasing the likelihood of peer influence on greater alcohol consumption.
BOTTOM LINE
- For individuals and families seeking recovery: This study shows that those most at–risk genetically for developing alcohol-related problemsmay be influenced by alcohol access, namely the fewer places in an area that sell alcohol, the fewer problems individuals with genetic liability will develop. Therefore, such individuals should consider the characteristics of the neighborhoods in which they live, particularly when relocating. If people have a choice between a town with a high vs low density of alcohol outlets, they may want to choose the town with the least access to alcohol if they want to lower the chances of developing an alcohol problem.
- For treatment professionals and treatment systems: Because those patients most at–risk for developing alcohol-related problems are also influenced by alcohol access, treatment professionals could recommend living spaces with fewer alcohol establishments for patients with current or the propensity to develop alcohol problems.
- For scientists: Gene-environment interactions in alcohol use disorders appear to be a prominent determinant of who will develop alcohol problems. Density of alcohol outlets is rarely considered in genetic/heritability studies of alcohol use disorders, and this measure may be a very important one to collect in future studies. Furthermore, when scientists analyze large databases, this information, if available, should be incorporated into analyses. Finally, when designing interventions, clinicians should be mindful of neighborhood alcohol characteristics and incorporate this into treatment and relapse prevention plans.
- For policy makers: This study indicates that those most at–risk for developing alcohol-related problems are likely to be highly influenced by alcohol access.Limiting the physical availability of alcohol to prevent easy access may reduce alcohol-related harm and has the benefit of being very cost-effective. The current study provides evidence suggesting that this strategy for reducing alcohol-related harm may be especially beneficial to those most at–risk for developing alcohol-related problems. In addition to availability, price of alcohol is the other big factor that influences consumption. To have major public health effects, lowering ease of access to alcohol through monitoring alcohol outlet density (e.g., granting fewer alcohol sales licenses),increasing alcohol cost (e.g., by adding an alcohol–specific tax), or introducing a minimum price per unit of alcoholmay reduce alcohol-related harms at the community level. This study could be relevant to the newly-emerging commercial cannabis industry as well. This data suggests that for those at–risk, more cannabis outlets may lead to more problems from cannabis use.
CITATIONS
Slutske, W. S., Deutsch, A. R., & Piasecki, T. M. (2018). Neighborhood density of alcohol outlets moderates genetic and environmental influences on alcohol problems. Addiction, 114(5), 815-822. doi: 10.1111/add.14534

