Behavioral treatments for youth with opioid use disorder – which approach works best?
Teens and young adults with opioid use disorder often receive treatments shown to be effective for other types of substance use disorders since there’s little scientific knowledge about what therapy approaches are most effective for this specific group of youth. In this study, authors used real-world treatment data to test how youth with opioid use disorder fared when receiving each of three common behavioral approaches.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Teens (age 12-17) and young adults (age 18-29) make up approximately 40% of substance use disorder (SUD) treatment seekers. However, treatment research largely focuses on samples of adults 18 and older, and even the young adult subset receives minimal focused attention within this larger group. As a result, there’s limited information available to guide treatment recommendations for a large subset of individuals who present for SUD treatment. While interventions such as the adolescent community reinforcement approach (A-CRA) have been developed for treating SUD during adolescence, little is known about the effectiveness of such specialized approaches for opioid use disorder.
There is also evidence that adolescents and young adults respond differently to SUD treatment compared to older adults. For example, among adults, younger age is a reliable predictor of early dropout from SUD treatment. There is also evidence that A-CRA specifically works better for adolescents compared to young adults. Adolescents and young adults with opioid use disorder differ from each other in important ways, as the transition from adolescence to young adulthood is characterized by increasing autonomy together with higher rates of substance use among peers. Given these key differences, interventions that are effective in general adult samples may work differently for these special populations. To help guide treatment recommendations for youth with opioid use disorder, Davis and colleagues compared the effectiveness of three common behavioral interventions for this understudied subset of patients, including A-CRA.
HOW WAS THIS STUDY CONDUCTED?
This was a quasi-experimental study of 785 adolescent and young adult participants who received one of three different behavioral outpatient treatments for opioid use disorder and were followed for one year, with assessments at treatment entry and three, six, nine, and 12 months later. The authors compared the groups on length of time before first opioid use in the year after presenting for treatment, using rigorous statistical control for group differences when participants entered treatment. Authors also compared findings for subgroups based on gender and age (i.e., tested whether gender and age influenced treatment effects).
The data for this study is from a large research project which collects data from SUD treatment facilities across the U.S. The authors identified 785 adolescents and young adults in the dataset who received one of three behavioral treatments for opioid use disorder between 2002 and 2013.
The first – cognitive behavioral therapy (CBT) – is a family of approaches which emphasize the importance of the relationship between thoughts, emotions, and behaviors. Some patients in the CBT group also received a brief intervention designed to increase motivation for change, known as motivational enhancement therapy (MET), though all participants receiving CBT were all grouped together including both those who did and those who did not receive MET as well. Second, the Adolescent Community Reinforcement Approach (A-CRA) is an adolescent-specific adaptation of a manualized cognitive behavioral treatment known as the Community Reinforcement Approach. A-CRA emphasizes building a rewarding life free of substance use, and actively engages parents or other caregivers in treatment. These two interventions, CBT and A-CRA, were compared to treatment–as–usual (TAU), or the facility’s typical treatment approach. TAU generally included components of 12-step facilitation, where providers systematically encourage patients to attend 12-step mutual-help meetings in the community, and case management. All participants met criteria for opioid use disorder using the project’s own measure, which uses a set of validated questions derived from Diagnostic and Statistical Manual of Mental Health Disorders (DSM-5) criteria.
Participants were followed for one year, with assessments at treatment entry and three, six, nine, and 12 months later. The primary outcome was participants’ self-reported time to first opioid use for each group in days after treatment entry. The authors also compared the effects of each treatment by age (adolescent vs. young adult) and gender to see if the treatments worked differently for teens vs. young adults and for females vs. males. To do this, the authors used a technique that yields an estimate of the likelihood at any given point during the study follow-up period that a participant who has maintained abstinence up to that point in time will use an opioid by the next time period (i.e., the next day). The authors also estimated likelihood based on age and gender subgroups within the overall sample.
The real-world setting of this study means that participants were not randomly assigned to the different treatments (a design known as “quasi-experimental”). Thus, treatment assignments may have differed based on factors that facilities use to make clinical decisions, which could also influence the study outcome. To address this, the study authors conducted a rigorous process of adjusting for factors that were different between the groups and might have explained any differences in outcomes. This improved their ability to say that the treatments themselves were responsible for group differences in time to opioid use.
The participants in this study were about 20 years old on average, and about a third of the sample (32.1%) were adolescents. Slightly less than half (42.7%) were female, and almost two-thirds (65%) were White. On average, participants reported using opioids approximately 30 of the 90 days prior to entering treatment. Most met criteria for a non-SUD mental health diagnosis, based on their clinician’s assessment, most commonly major depressive disorder (77.1%) or post-traumatic stress disorder (43.0%).
WHAT DID THIS STUDY FIND?
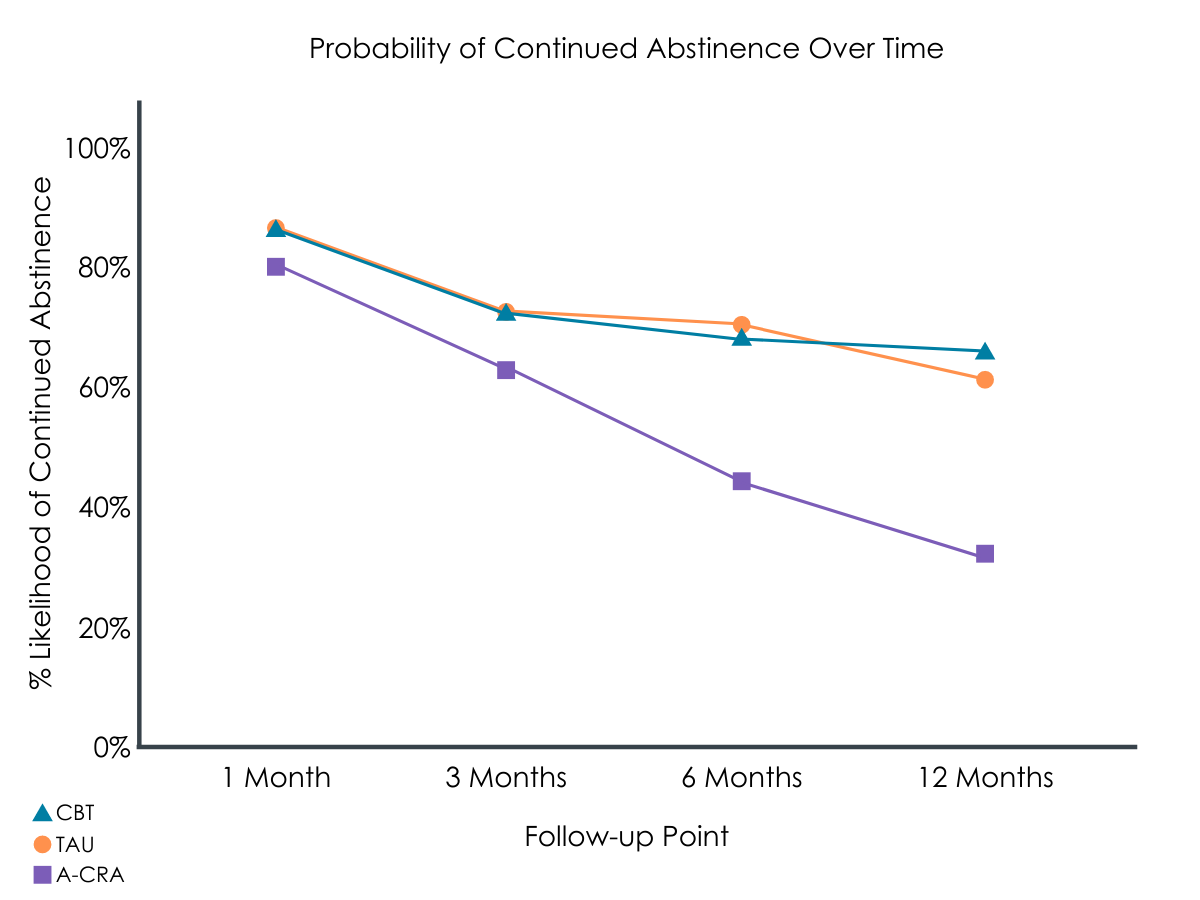
Figure 1. For individuals who are currently abstinent during the referenced points in time, this conveys the estimated chance that those individuals will remain abstinent over time.
Overall, adolescents and young adults receiving A-CRA were at much greater risk of returning to opioid use sooner than those who received TAU or CBT.
The A-CRA group was at 79% greater risk of returning to opioid use sooner during the follow-up period than the TAU group, and 122% greater risk compared to the CBT group. Regardless of treatment received, young adults were also more likely to use during the study period compared to adolescents, showing an increased risk of 79%. Females and males had a similar number of days to first opioid use after starting treatment.
Which treatment performed best was dependent on whether participants were teens or young adults, male or female.
Adolescent females appeared to benefit equally from all of the approaches considered in this study. When the authors compared risk for returning to opioid use during the follow-up period for this group, there were no significant differences between the interventions.
For adolescent males, CBT was the most effective, followed by TAU and A-CRA. Those receiving TAU were 155% greater risk of return to opioid use, while the A-CRA group showed a 214% increase compared to the CBT group.
Young adult females appeared to benefit most from TAU, followed by CBT and then A-CRA. TAU showed a 50% decrease in risk for return to opioid use compared to CBT, and a 130% decrease compared to A-CRA.
Young adult males benefitted most from CBT, followed by TAU and then A-CRA. The risk for returning to opioid use was 68% greater for TAU compared to CBT, and 208% greater for A-CRA.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Adolescents and young adults with opioid use disorder comprise a sizeable proportion of treatment seekers, though research to guide clinical practice has traditionally focused on adults. The authors of this study employed a rigorous methodological approach to compare naturalistically delivered behavioral treatments for a large national sample of youth with OUD. Their results showed that, overall, CBT and TAU – which generally consisted of systematic linkage to 12-step mutual-help meetings and case management – appear to work better than A-CRA in this sample, with some variation based on age and gender.
A-CRA was originally developed for treating cannabis use disorder, and previous work has shown that adolescents and young adults with opioid use disorder benefit less from this approach than peers with other primary SUD. The shorter length of abstinence for young adults compared to adolescents in this study also mirrors previous work showing that young adults with SUD benefit less from A-CRA than adolescents.
This study did not report which participants were also taking medications for opioid use disorder, an important component of effective treatment for opioid use disorder for some. During the period covered by the study (2002-2013) medications were used less frequently than they are today. For example, buprenorphine, one of the most common medications for opioid use disorder, was only approved by the FDA (for individuals 16+) in 2002. While research in this group is in its early stages, there is evidence that medications help youth stay in treatment. Youth are receiving medication for opioid use disorder less often than older adults, likely due to a variety of factors including limited research to inform safe practice guidelines as well as less positive attitudes towards medications among younger patients themselves. Future research should examine whether this study’s findings hold for youth receiving medication for opioid use disorder. Since a sizeable minority of patients opt out of medication when offered in general adult samples, future work should also compare response to behavioral treatments for medication and no-medication subgroups.
In this study, young adults fared worse than adolescents in treatment for opioid use disorder. Young adulthood is a unique period, when brain development is similar to adolescence, but environmental changes such as reduced parental supervision and reduced access to sober activities and peers present challenges for supporting abstinence. Thus, it may be necessary to develop treatment adaptations or specialized approaches for young adults in particular. Results from the female subgroups are also worthy of further examination, as females generally fared worse than males in treatment. Females who present for opioid use disorder treatment differ from males in a number of ways (e.g., higher likelihood of trauma experience), and it may be necessary to develop treatments which targets these unique challenges.
- LIMITATIONS
-
- The therapy in this study was not evaluated for content or fidelity to the treatments. As a result, it isn’t possible to know whether providers followed the CBT and A-CRA treatment manuals as intended by the developers. Furthermore, for TAU, which outperformed the other treatments for some subgroups, a broad variety of approaches may be included, and these likely varied by facility.
- While age and gender are important demographic characteristics for SUD treatment outcomes, this study did not (and likely could not, due to small numbers) incorporate other factors known to result in disparate SUD treatment outcomes, including racial/ethnic minority, socioeconomic status, and gender or sexual minority identity. Future work should continue examining the intersection of these key demographic factors.
- The study authors used a rigorous approach to address the effects of missing data in this naturalistic dataset (40% of participants were missing data by the 12-month timepoint, likely due to treatment dropout). However, one limitation in their approach is that participants who left the study did not contribute data. More traditional treatment research studies would typically treat such cases as if they had used opioids at the time that they stopped participating. While there is no perfect approach to managing missing data, this consideration is important for comparison of these findings with other research.
BOTTOM LINE
- For individuals and families seeking recovery: This study showed that CBT and treatments that link individuals systematically with 12-step mutual-help groups (“treatment as usual” in this study) appear to work better than A-CRA for adolescents and young adults with opioid use disorder, with some variation based on age and gender subgroups. However, because this study ended as medications for opioid use disorder were becoming more available, updated research would provide more definitive guidance on the best treatment approaches, including potential combinations of medication and behavioral treatment. When identifying a treatment facility for yourself or a loved one, broader features of the facility are the most important consideration, including whether evidence-based approaches such as CBT, A-CRA, or 12-step facilitation are offered. Family members who are experiencing the stress of an adolescent or young adult working to recover from opioid use disorder may also want to consider support for themselves.
- For treatment professionals and treatment systems: The results from this study showed that CBT and treatments that systematically link individuals to 12-step mutual-help (“treatment as usual” in this study) approaches as delivered in real clinical settings appear to be more effective than A-CRA for youth with opioid use disorder. Studies like this are important because youth respond differently to treatment compared to adults and are a sizeable portion of SUD treatment seekers. The authors of this study also found that young adults generally fared worse than adolescents, and females fared worse than males. This suggests a need for specialized approaches for young adults and female youth. Recommendations should be considered preliminary due to the absence of information on medication for opioid use disorder in the study sample. For facilities working to collect and evaluate outcomes for these interventions at the local level, these demographic factors may provide a useful reference point for patterns that may emerge within a treatment system.
- For scientists: This study examined hazard ratios for days to first opioid use among adolescents and young adults presenting for opioid use disorder treatment. Results showed that CBT and “treatment as usual” approaches that emphasize linking patients systematically with 12-step mutual-help groups appear to be more effective than A-CRA, with some variation among demographic (i.e., age and gender) subgroups. Differences in response for young adults and female patients also suggest that there is a need to identify strategies for better supporting these groups as they seek opioid use disorder treatment. This work will require replication and extension, as data collection ended in 2013, and the treatment landscape for opioid use disorder has shifted significantly since then. Specifically, research will need to examine the effects of behavioral treatments alone compared to combined medication and therapy to further inform treatment recommendations for youth with opioid use disorder.
- For policy makers: This quasi-experimental study used a large national dataset to examine the effects of different psychosocial treatments for opioid use disorder within a high-risk demographic group. Results showed that CBT and treatments that link individuals systematically with 12-step mutual-help groups (“treatment as usual” in this study) approaches as delivered in real clinical settings appear to be more effective than A-CRA for young adults and adolescents with opioid use disorder. Recommendations from these results should be considered preliminary, however, because the landscape of opioid use disorder treatment has changed since 2002-2013, with respect to the emphasis on (and availability of) opioid use disorder medications. Results showing that demographic sub groups respond differently to interventions illustrate the importance of making a variety of evidence-based approaches available and highlight the importance of funding research to inform treatment development for young adults and women. More broadly, this study illustrates the value of multisite efforts to collect and compile real-world clinical data. While such initiatives require significant resources in the form of increased effort and protected time for clinicians, they provide invaluable information to guide research and policy decision-making.
CITATIONS
Davis, J. P., Prindle, J. J., Eddie, D., Pedersen, E. R., Dumas, T. M., & Christie, N. C. (2019). Addressing the opioid epidemic with behavioral interventions for adolescents and young adults: A quasi-experimental design. Journal of Consulting and Clinical Psychology, 87(10), 941-951. doi: 10.1037/ccp0000406

