What Happens to the Brain During Recovery from Cocaine Use Disorder?
Substance use disorders are often accompanied by impairments to both brain structure and cognitive ability. This study examined how certain brain structures and their associated functions change with recovery from cocaine use disorder.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Brain imaging studies have repeatedly revealed altered brain structure among individuals with substance use disorder. Some structural abnormalities are seen across multiple substance use disorders (e.g., alcohol, cocaine, methamphetamine), including abnormalities of the prefrontal cortex. The prefrontal cortex is a structure composed of several sub-regions, all of which are implicated in various executive functions – a set of skills important for behavioral control and essential for addiction recovery (e.g., inhibiting behavioral responses to drug cues, implementing newly learned coping skills).
Addiction is frequently associated with reduced gray-matter volume (the density of brain cells) within these frontal regions, as well as impairment of the executive functions to which they contribute.
Importantly, research has begun to reveal what happens to the prefrontal cortex during recovery from substance use disorders and how it relates to executive cognitive abilities. Thus far, the majority of investigations addressing these issues have been cross-sectional in nature (e.g., assessment at one-time point).
Longitudinal studies that follow individuals with substance use disorder over time are needed to make stronger conclusions about whether neural and behavioral impairment is a predisposing factor that precedes addiction, or a consequence of repeated drug use. If neurobehavioral changes accompany addiction recovery, supporting their improvement during substance use treatment might benefit overall well-being and long-term recovery outcomes.
This study addressed this gap in the scientific literature by assessing whether individuals with cocaine use disorder after a period of remission (cessation of or significantly reduced cocaine use) showed increased gray matter volume in prefrontal cortex regions over time, and if these brain changes were associated with improved executive functioning.
HOW WAS THIS STUDY CONDUCTED?
Two groups were recruited from the New York Tri-State area and followed over 6 months.
- MORE ON STUDY METHODS
-
The first group was made up of 19 individuals (68% male; ~43 years old) diagnosed with cocaine use disorder (i.e. dependence; using the diagnostic and statistical manual of mental disorders, or DSM, 4th edition). All had recently attended or were currently attending one of three addiction treatment facilities and had at least 3 weeks of abstinence from all drugs. The second group consisted of 12 healthy controls (92% male; ~39 years old) who had no history of substance use disorder.
Both groups completed brain scans upon entering the study (i.e. baseline) and at a 6-month follow-up to assess gray matter volume changes over a 6-month period. Brain scans were performed with Magnetic Resonance Imaging (MRI), which produces detailed images of the brain that allow for the measurement of various structural attributes (e.g., size, shape, integrity) in specific brain regions. Participants also provided information regarding their substance use and mental health histories, and completed toxicology screens to assess recent drug use at baseline and follow-up.
In addition to these measures, the group diagnosed with cocaine use disorder completed neuropsychological tests that assessed a variety of executive functions, each of which is associated with distinct prefrontal cortex regions. Performed during both study sessions, these tests specifically targeted decision making skills (thought processes involved in selecting a choice from available options), conflict monitoring (detecting conflicts between behavioral goals and response tendencies/reflexes), cognitive control (ability to override impulses/habits and implement flexible, goal-oriented behaviors), and cognitive flexibility (the ability to adapt strategies/behavior to new environmental or situational cues).
Among recovering participants, duration of continuous cocaine abstinence averaged 149 days at baseline and 272 days at follow-up. On average, both groups were similar with respect to age, education, gender, and race. Relative to controls, the group diagnosed with cocaine use disorder had a greater proportion of nicotine users (84% vs. 50%) and reported more depressive symptoms as measured by the Beck Depression Inventory (although inventory scores suggested very few symptoms in both groups). Given the prevalence of smoking and psychiatric comorbidity among substance use disorder treatment-seeking populations, in general, these differences are not particularly surprising.
WHAT DID THIS STUDY FIND?
Among the cocaine use disorder group, gray-matter volume increased from baseline to follow-up in 3 prefrontal regions, including the:
- left inferior frontal gyrus
- left ventromedial prefrontal cortex
- right ventromedial prefrontal cortex
These regions can be seen in the figures below from the article.
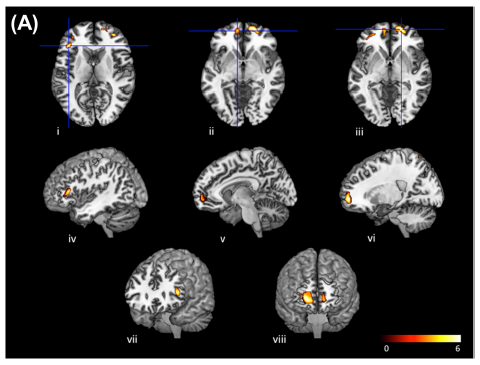
Images in the top row show the brain as if one is looking down at it from overhead. Images in the middle row show the brain as if one is looking at a left profile view of it at eye level. Bottom row images depict the brain head-on as if one is standing eye to ‘eye’ with it. The front of the brain (nearest to the forehead) is shown at the top most portion of the top row, the left most portion of the middle row, and at the central portions of the bottom row images.
Exploratory analyses indicated that this neural recovery occurred with remission, regardless of whether individuals remained abstinent over the 6-month period or experienced the occasional lapse (intermittent return to cocaine use). Thus, it may be that even reducing cocaine use can facilitate neural recovery.
No longitudinal changes in gray-matter volume were observed in the healthy control group, suggesting that brain changes were specific to those in remission from cocaine use disorder.
Neuropsychological performance in the cocaine use disorder group also improved from baseline to follow-up on two specific tasks, including:
- Wisconsin Card Sorting Task: assesses cognitive flexibility and is thought to recruit dorsal (top) and ventral (bottom) regions of the prefrontal cortex.
- Iowa Gambling Task: assesses decision making skills and is typically associated with activity in the ventromedial prefrontal cortex, among other frontal regions.
The authors found that improved performance on the Wisconsin Card Sorting Task was significantly related to increased gray-matter volume in the inferior frontal gyrus.
Although performance on the Iowa Gambling Task is traditionally associated with activity in the ventromedial prefrontal cortex, improved performance on this task was not significantly related to the increased gray matter volume seen in this region. Despite a non-significant correlation, it is interesting that improvement was seen both in ventromedial prefrontal cortex structure and associated neuropsychological functions of decision making, as measured by the Iowa Gambling Task.
WHY IS THIS STUDY IMPORTANT
Demonstrating recovery of not only brain structure, but also cognitive functions, suggests that individuals with substance use disorder can regain neurobehavioral functions that have been compromised after heavy and chronic drug use.
The finding of neurocognitive recovery during remission that was reported here suggests that prefrontal cortex alterations and associated cognitive difficulty may be at least partially attributable to cocaine, itself, rather than a predisposing factor that contributes to neurobehavioral alterations and the risk for developing addiction. Increased gray-matter volume of the prefrontal cortex has also been noted for individuals in recovery from alcohol and methamphetamine, in addition to cocaine. This opens doors for potential avenues of enhancing treatment for a variety of substance use disorders. Supporting neurocognitive recovery during addiction treatment might enhance long-term recovery outcomes.
With regard to the brain regions and respective executive functions that showed remission-related changes in this study, complementary treatments that aim to improve decision making skills and cognitive flexibility might aid implementation of newly learned skills important for maintaining sobriety. For example, encouraging the use of cognitive retraining games that target decision making skills could potentially accelerate their improvement, thereby making this skill set more readily available for treatment-seekers to select newly learned recovery-driven choices, and avoid harmful options, when making decisions. Indeed, the inferior frontal gyrus and ventromedial prefrontal cortex are prefrontal structures that are important for a variety of executive functions and their impairment might contribute to the maintenance of addictive behaviors. Thus, supporting the recovery of these structures and their functions with respect to cocaine use disorder might benefit addiction treatment outcomes.
One component of the study important to keep in mind is that individuals were using a range of substances in addition to cocaine, and some had additional mental health difficulties (e.g., anxiety disorders). The study, however, did not account for these individual differences, looking only at brain structure, cognitive performance, and cocaine remission. Although we cannot say with certainty that reducing/stopping cocaine use entirely accounts for the observed changes, this study does suggest that individuals recovering from substance use disorders can show neural and cognitive improvement. This study further demonstrated that neural recovery can occur even without complete abstinence, suggesting that positive recovery outcomes are also possible for individuals who struggle to maintain continuous sobriety, but who substantially reduce drug exposure.
- LIMITATIONS
-
- Although small sample sizes are common in neuroimaging studies, further research with larger sample sizes is needed to confirm and extend these findings. Additionally, the majority of participants in this study were male and African American. Sex and race differences merit further study, given genetic and environmental differences that can exist between groups and influence neurobehavioral outcomes. Whether or not these findings extend to women and individuals with other racial/ethnic backgrounds remains to be determined.
- Current comorbid psychiatric disorders were present in 32% of participants with cocaine use disorder at baseline. These conditions, including alcohol use disorder and post-traumatic stress disorder, are independently associated with alterations to frontal brain structures and functions. Although the incidence of these comorbidities did not change from baseline to follow-up, and multiple diagnoses are common among treatment-seeking populations, it is important to consider their potential influence on neurocognitive changes during addiction recovery.
- The overall range of cocaine abstinence durations were not reported. However, the statistics presented (e.g., standard deviations) suggest a lot of variability between treatment-seeking participants (i.e., some may have had just initiated abstinence while others had been abstinent for weeks or even months). Six-month trajectories of neurocognitive recovery are likely to differ between early and later abstinence periods. Thus, additional frontal brain regions and neuropsychological functions might have shown changes indicating recovery, had the sample been comprised only of individuals in the early stages of addiction recovery.
- Six of the 19 participants with cocaine use disorder remained in residential treatment throughout the entire study duration. Duration and quality of substance use treatment might play a role in neurocognitive outcomes – their influence on this study is not entirely clear.
NEXT STEPS
Additional longitudinal studies are needed to replicate these findings in individuals with cocaine use disorder who have a more restricted range of abstinence durations at baseline. Doing so can help us determine critical windows of recovery for brain structure and neuropsychological function during cocaine remission.
It is also important to determine if these findings are substance and/or cohort dependent – do these outcomes generalize to all individuals with substance use disorder or just apply to those with cocaine use disorder; do factors such as sex, race, abstinence duration, and psychological comorbidity influence recovery-based brain-behavior relationships? Furthermore, can social and environmental changes accelerate or otherwise affect the rate of brain-based recovery? Studying the association between all of these factors is sure to reveal a more comprehensive understanding of addiction recovery.
BOTTOM LINE
- For individuals & families seeking recovery: Studies that collect information about brain and behavior over time shed light on addiction recovery and help us to better understand what is involved in the recovery process – that together with the reduction or cessation of addictive behaviors and enhanced overall well-being, recovery can also occur in the brain, and translate to improvement in cognitive skills that play an important role in optimal behavior. This study provides early evidence that individuals with cocaine use disorder have the potential to at least partially reverse prefrontal cortex damage accompanying cocaine misuse, and regain associated cognitive abilities important for executive functions when cocaine use is stopped or significantly decreased.
- For scientists: This longitudinal investigation provides preliminary evidence that, for individuals with cocaine use disorder, significantly reducing or stopping cocaine use results in increased gray-matter volume in the inferior frontal gyrus and the ventromedial prefrontal cortex and improvement in associated executive functions over a 6-month period. These improvements suggest that executive dysfunction may be at least partially attributable to the deleterious effects of chronic, heavy cocaine use on the brain. Given the array of factors that can influence executive functions and their recovery, further investigation is needed to determine the components that underlie these neural and functional changes that occur during remission. It is also important to characterize the temporal trajectories of these neurocognitive improvements upon cessation of substance use. Identifying critical periods of neuropsychological recovery might inform future research on enhanced treatment interventions.
- For policy makers: Research studies like this one provide important information about the brain, behavior, and how it can change over time as a function of recovery from substance use disorders. This informs the types of cognitive functions that individuals with substance use disorder might show upon initiating remission and their potential for recovery over time. In the context of this study, executive functions (specifically cognitive flexibility and decision making) and the structures that contribute to them, including the inferior frontal gyrus and the ventromedial prefrontal cortex, have the potential to recover in individuals with cocaine use disorder during remission. These functions are essential to recovery, as executive dysfunction might contribute to disease progression and maintenance. Allocating funding to better understand the characteristics of executive function recovery and the brain changes that underlie behavioral improvement as they relate to substance use disorders might ultimately aid in the development of supplementary treatments that facilitate addiction recovery outcomes.
- For treatment professionals and treatment systems: This longitudinal study provides preliminary evidence of neurocognitive recovery among individuals with cocaine use disorder, not only in those who remain abstinent from cocaine, but also in those who significantly reduce cocaine use. More specifically, prefrontal cortex structural integrity and associated executive functions that play a key role in addiction maintenance and recovery, including decision making and cognitive flexibility, have the potential to improve with the cessation or reduction of drug use. Further research is needed to determine when these neural structures and behaviors begin to recover and how they translate to the broader trajectory of long-term remission. Nonetheless, studies like this one suggest that the consequences of long-term drug use on the brain and behavior can at least be partially reversed over time, perhaps even among patients presenting with more severe clinical profiles and/or higher incidence of relapse. When executive functions improve, there may be additional room for implementing more complex cognitive and behavioral treatments. Although it is yet to be determined, aiding the recovery of these skills with executive function retraining might be a feasible avenue for supplementary treatment in the future.
CITATIONS
Parvaz, M. A., Moeller, S. J., d’Oleire Uquillas, F., Pflumm, A., Maloney, T., Alia-Klein, N., & Goldstein, R. Z. (2017). Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: A longitudinal study. Addiction Biology, 22(5), 1391-1401.

