An up-to-date review of brain stimulation techniques for addiction treatment
Brain stimulation techniques show promise as new treatments for addiction. This report assesses their effectiveness at reducing craving and substance use by reviewing the scientific evidence published to-date.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Repetitive transcranial magnetic stimulation is a technique that painlessly activates (excitatory) or suppresses (inhibitory) activity in specific brain regions by sending short pulses of electrical current through the forehead. This technique has recently shown promise as an effective treatment for substance use disorder. By targeting regions in the brain that are thought to be associated with addictive behaviors (e.g., structures implicated in the brain reward pathway), this type of stimulation aims to fix imbalances in excitatory and inhibitory activity. For example, targeting frontal brain regions may help to reduce impulsive behaviors and reduce the motivation for substance use by strengthening or weakening connections between frontal regions and more distant brain structures like those involved in reward and motivation (e.g., the caudate nucleus). Given that this area of study is relatively new in the context of addiction, the authors of the current report conducted an up-to-date review of the current literature assessing transcranial magnetic stimulation as a treatment for substance use disorder symptoms.
HOW WAS THIS STUDY CONDUCTED?
The authors conducted a systematic literature review and meta-analysis (statistical analysis of many studies testing the effects of transcranial magnetic stimulation techniques on craving and substance use). All studies included in the review were randomized controlled trials comparing transcranial magnetic stimulation to either a control condition without stimulation or a control condition where participants received sham stimulation, a type of comparison condition where participants think they are getting the treatment being tested in order to account for improvement from simply expectations of improvement, often called the placebo effect. In transcranial magnetic stimulation trials, sham stimulation participants are meant to believe they are receiving the treatment, but either no brain stimulation occurs, or stimulation is applied to a brain region not directly related to addiction processes (e.g., motor cortex). Their literature review resulted in 26 randomized controlled trials of moderate to high quality.
Twenty-two of the 26 studies assessed the effects of excitatory (high frequency) stimulation, including 17 studies that concerned repetitive transcranial magnetic stimulation and five studies that concerned deep transcranial magnetic stimulation, which uses a different type of coil that is intended to target deeper brain structures (located more centrally in the brain) but in a more diffuse manner (has less specificity for the targeted brain region). These 22 studies examined both the left and right side of the brain in an area called the dorsolateral prefrontal cortex (a frontal brain region located near the forehead that plays a key role in reward processing, motivation, and behavioral control), as well as the insula (a deeper structure in the brain implicated in a broad range of addictive behaviors). Ten studies assessed the effects of inhibitory (low frequency) transcranial magnetic stimulation, using a variety of stimulation techniques and targeting different brain regions (see results). The total number of treatment sessions administered and the duration of treatment varied widely across studies, ranging from 270 to 20,000 pulses administered over the course of one to 16 treatment sessions.
A total of 748 drug or alcohol dependent adults (i.e., alcohol, nicotine, heroin, cocaine, methamphetamine, and cannabis dependence) were included across all studies included in the review. None of the participants had a co-occurring psychiatric disorder. The primary outcome was self-reported craving and the secondary outcome was substance use (measured using self-report or number of relapse cases). When possible, the authors also looked at the influence of other variables to better interpret the effect of the stimulation therapy, including the type of substance dependence (e.g., alcohol dependence, illicit drug dependence, nicotine dependence) and different stimulation methods used across reports.
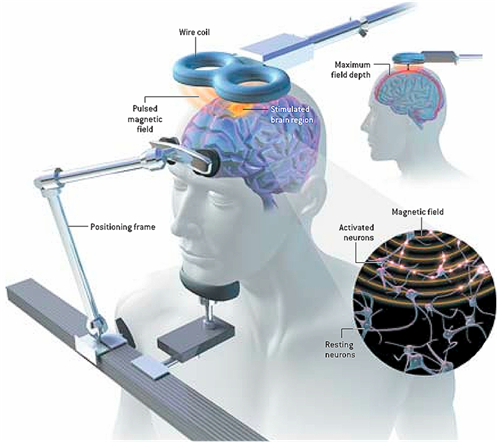
Figure 1. Repetitive transcranial magnetic stimulation: Activating or suppressing activity in a specific brain site by holding a magnet (AKA electromagnetic coil) against the head near that site and sending short pulses of electrical current through the magnet, which painlessly pass through the forehead and stimulate brain cells in the desired area. Common side effects of this non-invasive technique are relatively mild and include temporary headache, lightheadedness, scalp discomfort, tingling and/or twitching of muscles in the face.
WHAT DID THIS STUDY FIND?
Excitatory Transcranial Magnetic Stimulation (22 studies):
Excitatory Repetitive Transcranial Magnetic Stimulation (17 studies): Excitatory repetitive transcranial magnetic stimulation was associated with reduced craving and substance use.
Compared to a non-stimulation or sham stimulation condition, high frequency (excitatory) stimulation of the left dorsolateral prefrontal cortex (implicated in motivation and reward) stimulation was associated with significantly lower craving and reduced substance use (magnitude of effect: medium).
Analyses suggested that the total number of pulses administered to participants across all of their respective sessions predicted the magnitude of the anti-craving effect (i.e., more total pulses administered associated with less craving). Among the three studies that reported follow-up data (average follow up at four months), analyses suggested that this stimulation did not have a lasting effect on craving. Importantly, substance appeared to play a role in the magnitude of the stimulation’s effect on craving; the most robust effect was seen for illicit drug dependence (large effect), followed by nicotine dependence (medium effect), and alcohol dependence (small effect). When the authors assessed studies of the right hemisphere, they found no significant anti-craving effect of high frequency stimulation in the right dorsolateral prefrontal cortex (implicated in self-control and withdrawal related behaviors).
Excitatory Deep Transcranial Magnetic Stimulation (5 studies): Excitatory deep transcranial magnetic stimulation was associated with reduced substance use.
Compared to a non-stimulation or sham stimulation condition, excitatory deep transcranial magnetic stimulation of the left and right dorsolateral prefrontal cortex and the insula significantly reduced substance use. Conversely, excitatory deep transcranial magnetic stimulation of the medial prefrontal cortex (implicated in arousal, as well as automatic and impulsive behaviors) did not have a significant effect on substance use, when compared to control conditions. This method of stimulation did not have an effect on craving, regardless of the brain region targeted.
Inhibitory Transcranial Magnetic Stimulation (10 studies):
Inhibitory stimulation did not have a significant effect on craving or substance use.
Regardless of the stimulation technique administered or brain region targeted, inhibitory stimulation did not affect craving and/or substance use outcomes. These outcomes included: 1) Repetitive low frequency stimulation of the right or left dorsolateral prefrontal cortex (4 studies), or the medial prefrontal cortex (4 studies) with no effect on craving, and 2) inhibitory deep transcranial magnetic stimulation of the right and left dorsolateral prefrontal cortex and insula (2 studies) with no effect on craving or substance use.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This meta-analysis highlights the potential for non-invasive brain stimulation techniques in the treatment of substance use disorders. However, the effectiveness of stimulation appears to depend on the type of transcranial magnetic stimulation applied, with excitatory repetitive transcranial magnetic stimulation showing the most promise for alleviating substance use disorder symptoms.
Figure 2.
The author’s findings are in line with another recent meta-analysis, hich also suggested the anti-craving effects of high frequency repetitive transcranial magnetic stimulation. The current meta-analysis adds to prior findings by suggesting that high frequency repetitive transcranial magnetic stimulation, specifically of the left dorsolateral prefrontal cortex, may yield the greatest effect on craving. Despite a robust effect immediately after stimulation, outcomes suggested that the benefits of stimulation may not be retained over time. However, studies included in this meta-analysis had widely varying brain stimulation methods (total number of stimulation sessions ranged from one to 16; total number of pulses administered ranged from 270 to 20,000). Furthermore, only three studies provided follow-up data. Therefore, additional research is needed to identify the optimal treatment duration and to better understand how long these effects last beyond the final treatment episode. The authors’ analysis further suggests that high frequency repetitive transcranial magnetic stimulation in the left dorsolateral prefrontal cortex may be most beneficial for individuals with illicit drug use disorders, with this cohort showing the most robust (large) anti-craving effect.
Although this stimulation method did not have a significant effect on craving when administered in the right dorsolateral prefrontal cortex, half as many articles reported on this brain region, and substance use outcomes were not assessed in this context. Conversely, a previous review found a larger effect of repetitive transcranial magnetic stimulation on craving/substance use when administered to the right dorsolateral prefrontal cortex. Conflicting findings may be due to a limited literature and varying methods across brain stimulation studies and reviews. The current review also found no significant effect of inhibitory stimulation on craving or substance use. But again, methodologies and study populations of interest widely varied between reports which limits interpretation of its effectiveness. Taken together, this meta-analysis along with previous reviews further highlight the need for additional investigation to better understand the potential therapeutic effects of inhibitory stimulation, as well as excitatory transcranial magnetic stimulation of the right hemisphere.
Nonetheless, excitatory transcranial magnetic stimulation shows promise for treating substance use disorder symptoms. In addition to revealing the benefits of high frequency repetitive transcranial magnetic stimulation, this meta-analysis suggests the benefits of deep transcranial magnetic stimulation. This type of stimulation can reach deeper brain structures (structures more centrally located and further from the scalp) and might enhance dopamine activity in the brain, which is thought to be deficient in individuals with substance use disorder. Although the exact mechanism of its benefits is not fully understood, this report showed that deep transcranial stimulation significantly reduced craving and substance use when applied to the right and left dorsolateral prefrontal cortex and the insula. Given that the use of excitatory transcranial magnetic stimulation for treating substance use disorders is relatively new, future research will help determine its full potential and underlying mechanisms.
- LIMITATIONS
-
- Study populations with co-occurring psychiatric disorders were excluded from this meta-analysis. Given that about 50% of individuals who meet criteria for substance use disorder in the past year also present with a co-occurring psychiatric disorder, outcomes from this report may not apply to all substance use disorder populations.
- Although the outcomes suggest the superior effects of left dorsolateral prefrontal cortex (DLPFC) stimulation, the majority of studies looking at left DLPFC focused on illicit drug or nicotine use disorders. Furthermore, the majority of studies looking at the right DLPFC concerned alcohol use disorder and substance use disorder severity was not evaluated. Therefore, substance type and disorder severity could influence these outcomes and additional research is needed to make conclusions about the effectiveness in different brain hemispheres and in different substance use disorder cohorts. The current report did not examine the duration of time over which stimulation sessions were administered, requiring further assessment of the influence of treatment schedule.
- Assessment of inhibitory stimulation was limited to 10 studies, which used a broad range of stimulation techniques and focused on different substance use disorder populations. Given the small number of studies implementing inhibitory stimulation, the authors were unable to assess the impact of stimulation type and substance. Furthermore, only 3 studies reported follow-up data, with the average follow-up occurring 4 months after stimulation. Although exploratory assessment in this report suggested no lasting effect of stimulation on anti-craving. Additional research is needed to determine the factors that influence inhibitory stimulation outcomes and whether this type of stimulation can be beneficial for certain cohorts and have lasting effects.
BOTTOM LINE
- For individuals and families seeking recovery: Brain stimulation techniques are a relatively new and promising therapeutic technique for treating addiction. By non-invasively stimulating brain areas associated with addiction and reward, we may be able to help some individuals change addictive behaviors. This review confirms the effectiveness of short-term brain stimulation for reducing substance use and craving, and goes one step further by suggesting that it may be most effective in frontal brain regions associated with motivation and reward. These benefits may vary by substance, with illicit substance use disorders (e.g., heroin, cocaine) showing the greatest response to brain stimulation. Still, this area of study is new, and more research is needed to identify which brain stimulation methods can target different addictive behaviors, and whether these effects last beyond the first few weeks after receiving the treatment. Individuals interested in trying brain stimulation therapies are encouraged to contact their health insurance providers and inquire about whether or not these services are offered and covered by their plan.
- For treatment professionals and treatment systems: Existing research suggests that stimulating brain regions associated with addictive behaviors may help alter brain activity and help prevent craving and substance use. This review highlights the potential therapeutic befits of specifically stimulating left frontal brain regions associated with motivation and reward and suggests this effect may be most robust for illicit substance use disorders as opposed to alcohol or nicotine use disorders. Although excitatory brain stimulation techniques seem to produce positive outcomes, this review also highlights the lack of longitudinal research and variability in the methods employed across studies conducted thus far, which calls for additional investigation before this non-invasive technique is used in a clinical setting.
- For scientists: This meta-analysis complements previous reviews, suggesting the anti-craving and substance-use reduction effects of high frequency transcranial magnetic stimulation in the treatment of substance use disorder. It also furthers prior reports by proposing the superior effectiveness of brain stimulation in the left dorsolateral prefrontal cortex, suggesting a more robust effect for illicit substance use disorders (as opposed to alcohol and nicotine), and revealing the potential influence of total pulses administered on the magnitude of the anti-craving effect. However, this review highlights the need for additional longitudinal research to assess the longevity of these effects. Given the heterogeneity of low frequency transcranial magnetic stimulation studies and the potential confounding effect of substance use disorder type on hemisphere-related outcomes, further investigation in these areas is also encouraged. Additional research is also needed to determine the potential additive effects of transcranial magnetic stimulation when combined with other behavioral/medication therapies, and to assess whether or not this technique is effective for individuals with common comorbidities. Examining the neurobiological mechanisms that underlie these effects will ultimately help determine the full potential of stimulation techniques for aiding addiction treatment and might also facilitate identification of transdiagnostic neurobiological processes that underlie multiple psychiatric disorders.
- For policy makers: Repetitive transcranial magnetic stimulation is a non-invasive technique that has recently shown promise as an effective treatment for substance use disorder. By targeting regions in the brain associated with addiction, brain stimulation techniques have the potential to fix imbalances in brain activity and facilitate recovery by reducing substance use and craving. This review reiterates their potential but also underscores the need for additional research before brain stimulation techniques can be implemented clinically. Additional funding is needed to explore the duration of the treatment’s effects and which stimulation methods are most effective for different substance use disorder populations. Investigating therapies like these could ultimately lead to effective, non-invasive, and inexpensive options for supporting addiction treatment.
CITATIONS
Zhang, J. J., Fong, K. N., Ouyang, R. G., Siu, A. M., & Kranz, G. S. (2019). Effects of repetitive transcranial magnetic stimulation (rTMS) on craving and substance consumption in patients with substance dependence: a systematic review and meta‐analysis. Addiction, 114(12), 2137-2149. doi: 10.1111/add.14753

