Does Gender Impact Treatment Retention for Individuals with Substance Use & Mental Health Disorders?
For residential treatment settings, treatment retention is a key factor in the recovery process as longer length of stay predicts more favorable outcomes including lower rates of post-treatment substance use and lower rates of readmission. While gender itself does not predict retention, previous studies have pointed to differences by gender between factors that influence retention.
Morse and colleagues examined patient-level characteristics by gender to identify factors that predict treatment retention (measured as treatment days since baseline interview) in a private residential treatment facility for patients with co-occurring mental health and substance use disorders.
The sample was comprised of 1317 consenting participants who voluntarily sought residential treatment at one of the three facilities operated by Foundations Recovery Network, a private for-profit treatment provider located in Memphis, Tennessee, Malibu, California, and Palm Springs, California. All data was collected through assessments with Masters’ level clinicians. Overall, participants were demographically representative of patients attending treatment at these facilities during this time period.
95% (n = 778) of participants were male and 41% (n = 539) were female. Significantly more women were Caucasian (94%) than men (88%). Women were significantly older than men (36 years and 38 years, respectively). A significantly greater proportion of men (vs. women) were employed in the last 30 days (60% and 46%, respectively)
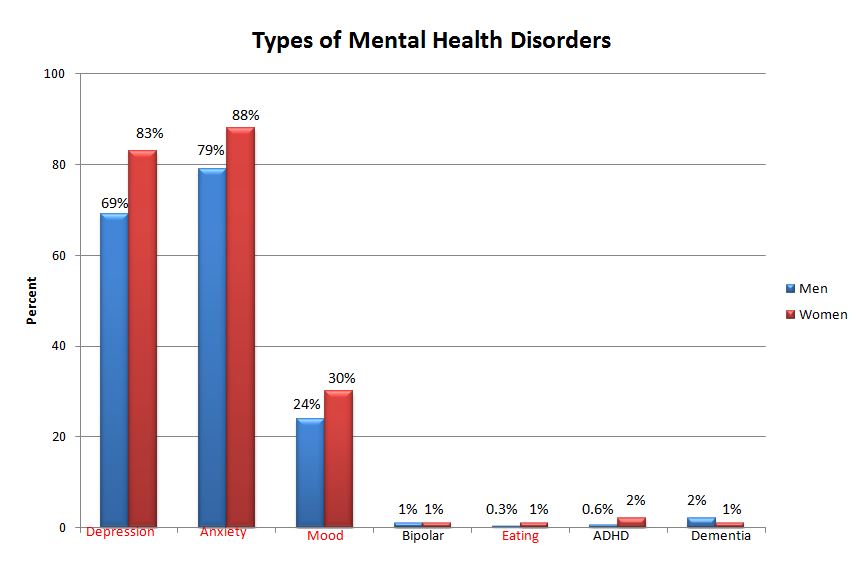
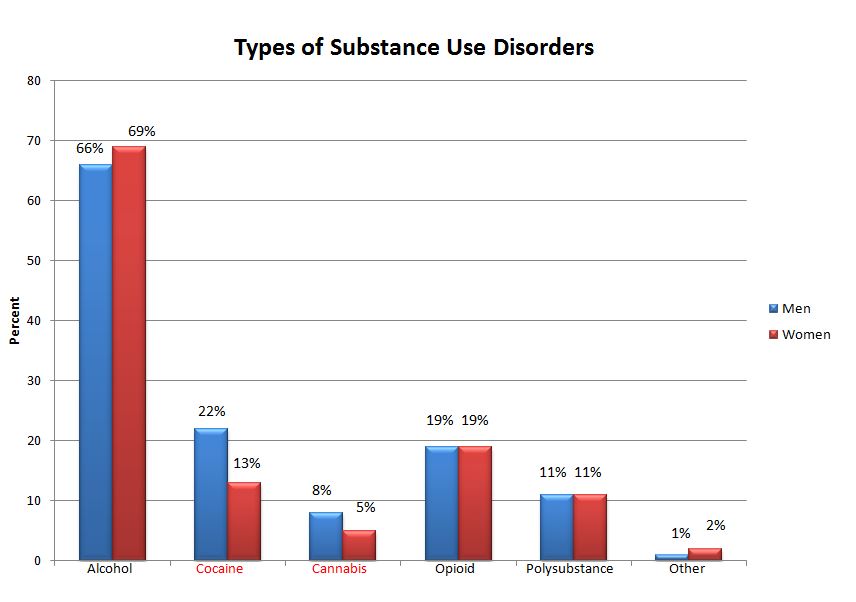
There were significant differences in 6 of the 7 Addiction Severity Index (ASI) subscales with women reporting higher (i.e., more severe) scores in the areas of medical, employment/support, family/social relationships, and psychiatric issues, and men reporting higher scores in the drug and legal subscales.
Men had significantly higher University of Rhode Island Change Assessment (URICA) scores in the precontemplative stage than women, meaning that more women were in a stage that represented greater readiness for change in their substance use.
While the expected length of stay (LOS) is 28 to 40 days, recommended LOS was based on individual assessment. The average LOS for men (30 days) was significantly different than LOS for women (35 days). 48% of women and 41% of men were retained in treatment at day 30. While this dichotomous outcome of retention (i.e., staying in treatment for 30 days or not) did not result in a significant difference by gender, the trajectories of treatment retention by gender (shown in the figure below) were significantly different.
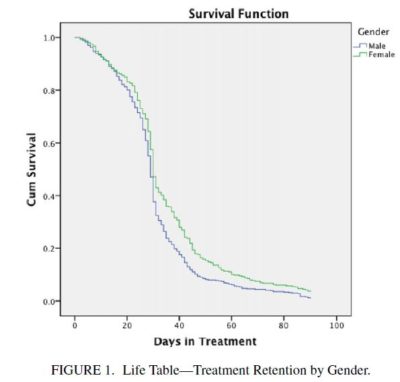
Source: (Morse et al. 2015)
The authors then used Cox proportional hazards regression with a model for each gender to assess which factors predicted treatment retention.
- For men, an ADHD (vs. mood disorder) diagnosis (Hazard ratio [HR]: 4.61) and ASI employment score (HR: 0.58) were significantly associated with the outcome. Men with ADHD diagnosis were 4.6 times more likely to be retained in treatment longer than men diagnosed with a mood disorder, and men with a higher ASI employment score (i.e., more severe employment issues) were less likely to remain in treatment longer.
- For women, cocaine (vs. alcohol) use (HR: 0.58), depression (vs. mood disorder) (HR: 1.93), ASI alcohol score (HR: 1.56), and readiness to change (precontemplative [HR: 0.68] or contemplative [HR: 0.58] stages on URICA) were significantly associated with greater likelihood of remaining in treatment. This means, for example, that women who used cocaine were 42% less likely to remain in treatment longer than women who used alcohol, and women with a diagnosis of depression were 93% more likely to remain in treatment longer than women diagnosed with a mood disorder.
IN CONTEXT
This study explored the effects of gender on factors that predict treatment retention among patients with co-occurring substance use and mental health disorders in three private, residential facilities.
As shown by the high ASI composite scores, women entered treatment with greater severity of issues relating to medical, employment/support, family/social relationships, and psychiatric measures than men. Because of these high scores and their possible association with greater motivation and readiness for change, women tended to stay in treatment an average of 5 days longer than men.
- LIMITATIONS
-
- While this increased LOS may be attributed to the factors found to be significant in the analysis, it is difficult to interpret these results with certainty due to issues with classification of the variables. For example, the category for mental health disorders in the study included major depression, bipolar disorder, and mood disorders, though diagnostically, mood disorders subsume the more specific major depressive disorder and bipolar disorder. This methodological nuance reduces the confidence in, and in parallel, clinical application of, the regression analysis as some patients may be misclassified or could fall into multiple categories.
- Low numbers of participants within certain categories (e.g., only 4 out of 778 men had ADHD) may have resulted in a biased estimate from the Cox proportional hazards models.
- While this study raises important questions for the treatment of patients with co-occurring disorders, there are other variables to consider such as the private treatment facility setting. Since patients may be responsible for some out-of-pocket spending (e.g., co-pays or deductibles), it is important to consider how this influences ability to stay in treatment. For example, a person whose insurance policy only covers a certain amount of time in treatment may be forced to leave despite their desire to stay. Additionally, since all participants voluntarily entered treatment, this study may represent a population that is inherently more motivated. It is important to consider facility-level factors in addition to patient-level factors when addressing the barriers and facilitators of remaining in care.
BOTTOM LINE
- For individuals & families seeking recovery: Since different factors may impact treatment retention by gender, there may be potential value in attending treatment that considers the specific experiences of women and men.
- For scientists: More evidence is needed to evaluate the differences in treatment retention by gender for patients with co-occurring substance use and mental health disorders. More rigorous methods should be used to examine the effects of gender on treatment retention.
- For policy makers: As there is still uncertainty surrounding this issue, more evidence is needed before policy changes regarding gender-based treatment services for people with co-occurring disorders are put into place.
- For treatment professionals and treatment systems: When treating a patient, it may be important to recognize how their needs may vary by gender.
CITATIONS
Morse, S. A., MacMaster, S., Choi, S., & Adams, S. M. (2015). Gender Differences in Treatment Retention Among Individuals with Co-Occurring Substance Abuse and Mental Health Disorders. Substance use & misuse.

