Study finds that cannabidiol (CBD) reduces drug craving and anxiety in patients recovering from heroin use disorder
The widespread use of heroin and prescription opioids in the United States during the past decade has resulted in an unprecedented epidemic of opioid addiction, and few treatments for heroin use disorders are currently available. In this study, authors conducted a clinical trial to test whether cannabidiol (CBD), a non-intoxicating cannabinoid that is found in the cannabis plant, could reduce drug craving and anxiety in recently-abstinent individuals with heroin use disorder. The study found that, compared to those who received a placebo, individuals who received a dose of CBD medication showed a reduction in craving for heroin as well as reduced anxiety, which lasted for about a week after taking the CBD medication.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
In the past decade, there has been an unprecedented spike in opioid use disorder, which has led to more than 300,000 opioid-related deaths in the United States. Opioid use disorder medications such as methadone and buprenorphine (often prescribed in a formulation with naloxone, known by the brand name Suboxone) help reduce opioid use and reduce risk for opioid-involved overdoses. In some areas, however, these medications are often underutilized and therefore can be difficult to access, creating a treatment gap in which those who need medications face barriers to actually receiving them. Further, 20-40% of opioid use disorder patients do not want to take agonist treatments.
One of the hypothesized factors contributing to these barriers is that methadone and Suboxone can be misused or diverted because they can produce euphoria. Consequently, discovering effective alternative medications that can also treat opioid use disorder that circumvent concerns about their psychoactive properties could help more of those affected. To address this problem, the authors investigated whether the cannabinoid, CBD, which is thought to be safe and non-addictive, could be useful in the treatment of opioid use disorder.
HOW WAS THIS STUDY CONDUCTED?
This was a randomized clinical trial with 42 participants who received one of two different CBD medication doses or a placebo once daily for 3 days and were then exposed to drug-related or neutral cues to see whether CBD could reduce opioid cravings and anxiety – factors strongly associated with relapse to opioid use.
Participants were recruited through advertisements. Most participants indicated preference for intranasal heroin use, most reported currently using more than 10 bags of heroin (one bag = 1 g) daily, and on average, participants had been using heroin for over 10 years. The majority of participants (64.3%) had been abstinent from heroin use for less than 1 month.
The study medication used in this study, EPIDIOLEX, is an FDA-approved medication that is dispensed through a pharmacy (not to be confused with “medical marijuana,” which is comprised of a wide variety of non-federally-regulated cannabis projects). EPIDIOLEX is a plant-derived CBD liquid formation. Participants were randomly assigned to receive 400 mg of CBD, 800 mg of CBD, or a placebo medication. CBD or placebo was administered once daily for 3 days. In addition to measuring the effect of the medication on opioid craving, anxiety, the authors also collected measures of positive and negative emotions, vital signs (skin temperature, blood pressure, heart rate, respiratory rate), and salivary cortisol levels, which measure stress response.
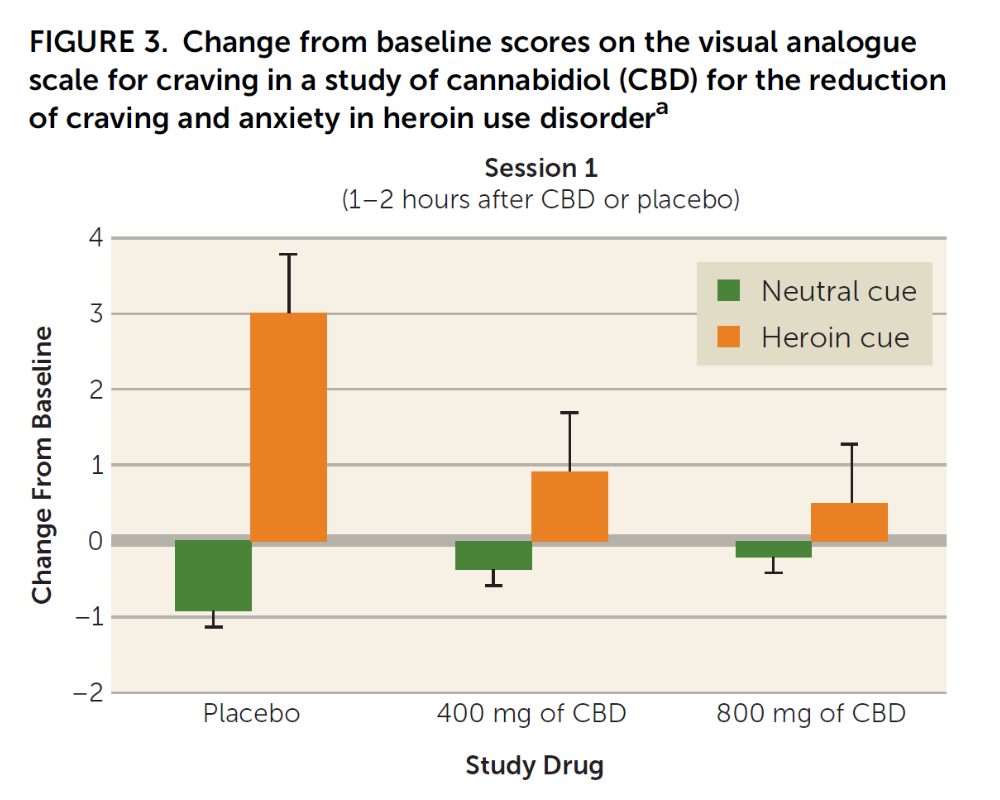
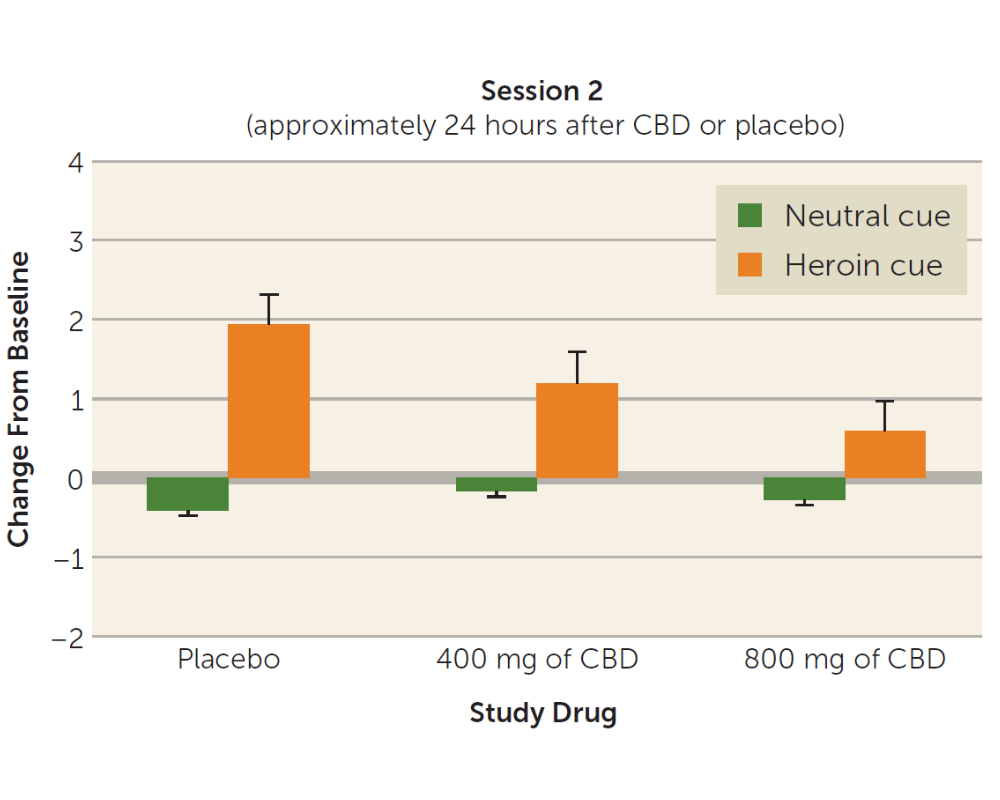
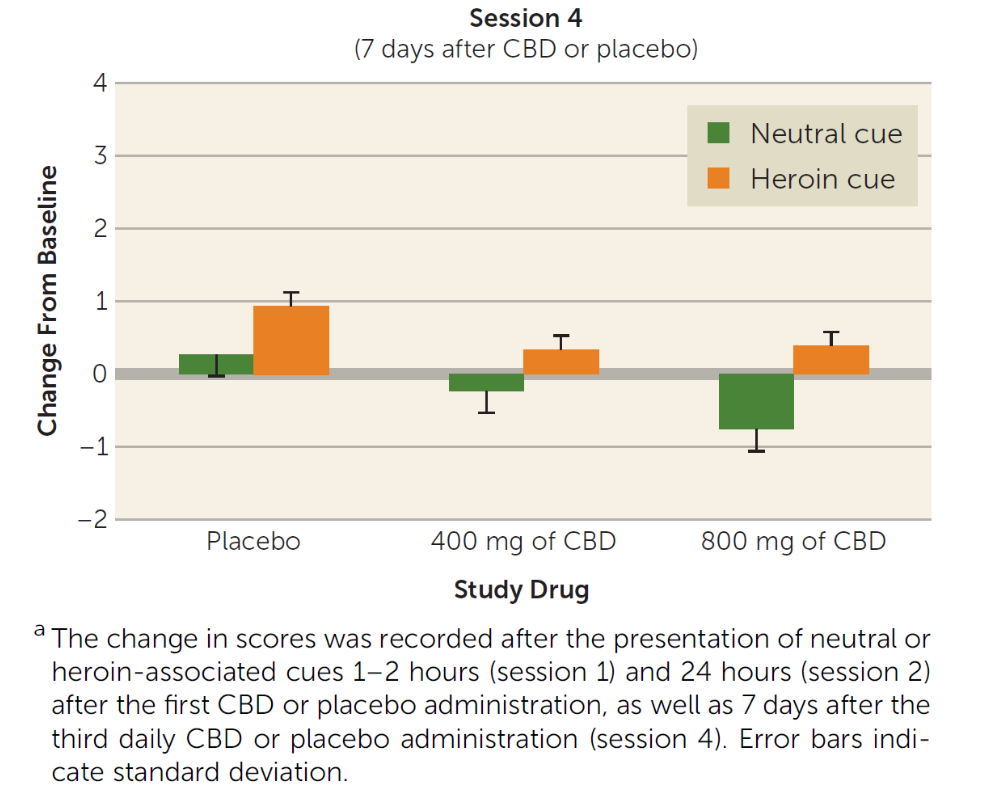
At three time points – immediately after the CBD or placebo administration; 24 hours after the CBD or placebo administration; and 7 days after the third and final CBD or placebo administration – participants were exposed to drug–related and neutral cues. The 3-minute neutral cue condition consisted of a video showing relaxing scenarios, such as scenes in nature. The drug cue condition was a 3-minute video that showed intravenous or intranasal drug use, depending on the participant’s reported preferred route of drug use. Immediately after the presentation of the videos, participants were also exposed to neutral objects or to heroin–related paraphernalia (e.g., syringe, rubber tie, and packets of powder resembling heroin) for 2 minutes. Authors examined whether patients who received CBD, compared to those who received placebo, showed differences in opioid craving, anxiety, positive and negative emotions, or vital signs, after being exposed to the drug or neutral cues.
WHAT DID THIS STUDY FIND?
Individuals receiving the non-psychoactive cannabinoid CBD medication reported less craving after being exposed to drug cues compared with individuals receiving placebo. This effect lasted at least a week after the CBD or placebo administration, when individuals receiving the high-dose of CBD (but not the low-dose) still reported less craving compared with those receiving placebo. In addition, CBD reduced measures of stress response after the drug cue – such as heart rate and salivary cortisol increases. Individuals receiving CBD reported less anxiety after being exposed to drug cues compared with individuals receiving placebo (though there were no significant differences in anxiety between participants receiving the low-dose vs. the high-dose of CBD). There was no effect of CBD on positive affect or on any cognitive measures.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
In light of the opioid epidemic, it is important to identify as many strategies as possible to curb opioid addiction. In the past few years, scientists have asked whether or not cannabis use can help individuals recover from opioid use disorder or may serve as a less-risky pain management approach to pharmaceutical opioids. Individuals also report using cannabinoids in an effort to cut back or quit other substances, but currently, data do not support this indication. Some studies have shown no benefit; in fact, studies have shown that cannabis use is related to greater odds of both new-onset opioid use and opioid use disorder 3 years later. The small, experimental study here shows a potential benefit of CBD in reducing cue-induced craving and anxiety in heroin-abstinent individuals. This suggests a potential role for CBD in relapse prevention of heroin use disorder. This study takes a more rigorous approach that can serve as a model for future studies of cannabinoids and their potential role in OUD treatment and recovery.
- LIMITATIONS
-
- The sample size in this study was very small and, although results are promising, the findings need replication in larger samples. The small sample also did not allow for exploration of sex/gender effects, which could be important given that women typically have higher craving and anxiety than men.
- The study medication used in this study, EPIDIOLEX, is an FDA-approved medication that you can only get from a pharmacy. Though EPIDIOLEX is derived from cannabis, it is NOT medical marijuana. This medication does not contain THC, which is the compound in the cannabis plant that causes the ‘high’ and euphoria. It is therefore important for patients to realize that although benefits of CBD were found, this study does NOT support the use of “medical marijuana” for opioid use disorder.
- This study only examined opioid craving for 7 days. It is still unknown if CBD would reduce opioid craving past the 7-day window examined in this study or whether use of CBD actually translates into less use of actual opioids.
- Patients in this study had to be abstinent from opioids, and not taking any agonist therapies. Therefore, the population in this study represents individuals who are doing well and may respond will to lots of different interventions. However, this population may not be representative of opioid use disorder patients more generally.
BOTTOM LINE
- For individuals and families seeking recovery: This study showed that compared to placebo the non-psychoactive cannabinoid, CBD, was associated with substantially decreased cue-induced craving and anxiety for those with heroin use disorder. Many individuals with opioid use disorders are seeking alternative treatments to curb cravings and reduce anxiety, and many are reluctant to try agonist treatments such as methadone or suboxone. While more research is needed to flesh out whether CBD increases the likelihood of long-term abstinence, this study suggests individuals may benefit from EPIDIOLEX, the FDA-approved CBD medication, but more larger studies are needed to confirm this. It is important to note, however, that individuals are using cannabis in its unregulated forms, and legislatures are passing medical cannabis laws that identify opioid use disorder as one of the conditions for which cannabis is indicated without evidence to support this indication. Consequently, individuals seeking to use cannabis, in general, for opioid addiction should proceed cautiously.
- For treatment professionals and treatment systems: This study showed that compared to placebo, CBD was associated with substantially decreased cue-induced craving and anxiety for those with heroin use disorder. A recent survey found that a considerable percentage (30%) of individuals receiving agonist treatment were worried about encountering negative attitudes related to being prescribed agonists, and only 33% reported their provider discussed this with them prior to attending a meeting. If CBD does pan out as a potential treatment of heroin use disorder, this could appeal to many patients, and could be a good complement to recovery support services. It is important for treatment professionals to be aware that the unregulated forms of cannabis, e.g., those that can be purchased at medical marijuana dispensaries, are still unproven treatments, and may in fact produce more harm than good.
- For scientists: This study showed that compared to placebo, CBD was associated with substantially decreased cue-induced craving and anxiety for those with heroin use disorder. More work is needed that more precisely measures whether CBD increases the likelihood of long-term abstinence, as well as for whom, and under what conditions, this medication work best. Greater knowledge in this regard could inform the nature of medication development more broadly. By pursuing investigation into other alternative treatments for opioid use disorder, scientists may be able to help reduce stigma and improve outcomes for patients with OUD.
- For policy makers: This study showed that compared to placebo CBD was associated with substantially decreased cue-induced craving and anxiety for those with heroin use disorder. While more research is needed, CBD may be an alternative to other medications for opioid use disorder, which are limited and not well-accessible to racial/ethnic minorities and those without financial means. Policy makers, however, should be aware that this study does not provide evidence that unregulated forms of cannabis, especially those containing THC, help with OUD. Funding research studies that examine pure forms of CBD, and other alternative treatments for opioid use disorder, could help improve outcomes and reduce the public health burden of the current epidemic of opioid addiction.
CITATIONS
Hurd, Y. L., Spriggs, S., Alishayev, J., Winkel, G., Gurgov, K., Kudrich, C., . . . Salsitz, E. (2019). Cannabidiol for the reduction of cue-induced craving and anxiety in drug-abstinent individuals with heroin use disorder: A double-blind randomized placebo-controlled trial. American Journal of Psychiatry, (ePub ahead of print). doi: 10.1176/appi.ajp.2019.18101191

