Contingency Management + Parent Participation = Further Benefits to Adolescents?
Clinical addiction research has received much support for marijuana related studies given the field’s limited knowledge in the face of the changing sociopolitical landscape for marijuana medicalization and legalization.
However, there already exists a sizeable body of evidence documenting marijuana’s harm on adolescent functioning, including psychiatric problems, academic performance, and risky sexual behaviors as well as emerging data on its negative impact on brain development.
Developing, testing, and implementing effective treatments for adolescents with cannabis use disorders (CUD) are of particular public health significance now, given this changing landscape which is likely to increase marijuana availability, adolescent exposure, and therefore, increased prevalence of CUD.
Stanger and colleagues tested whether adding contingency management (CM) to one of the current state-of-the-art treatments, motivational enhancement plus cognitive behavioral therapy (MET/CBT), would improve outcomes among 153 adolescents with a cannabis use disorder.
Contingency management (CM) is one of the gold standard treatments for adolescents, and incorporates techniques that give patients rewards for enacting a recovery behavior such as attending treatment or for staying abstinent and producing a negative urine toxicology screen.
More specifically, MET/CBT (n = 51) was compared to MET/CBT+CM (n = 51), as well as to MET/CBT+CM and a parent skills training approach (MET/CBT+CM+parent involvement (PT); n = 51), during a 14-week intervention period including twice weekly toxicology screens, and 3-month, 6-month, 9-month, and 12-month follow-ups. For the CM, adolescents received gift cards for negative toxicology screens during weeks 3 to 14 (maximum of $590 during treatment).
In addition, at least one adolescent caregiver was trained in home-based CM where they were counseled to provide rewards for abstinence and negative consequences for substance use, including a take-home saliva test to assess for recent alcohol use.
Incentives were also available for up to 3 months after the index treatment episode (i.e., continuing care) in response to weekly negative toxicology screens. MET/CBT participants received smaller rewards for completing urine toxicology screens (irrespective of whether they were positive/negative).
In PT, parents worked weekly with a therapist during the index treatment episode to target their child’s problem behaviors other than substance use.
The sample was 89% male, 62% African American, and between 12 and 18 years of age with an average age of 16. Regarding co-occurring psychiatric disorders, patient report showed approximately 25% with oppositional defiant and/or conduct disorder (ODD; CD), 15% with attention-deficit/hyperactivity disorder (ADHD), and 15% with major depressive disorder (MDD). Parent reports were higher for ODD/CD and ADHD, but similar for MDD.
Source: (Stranger et al., 2015)
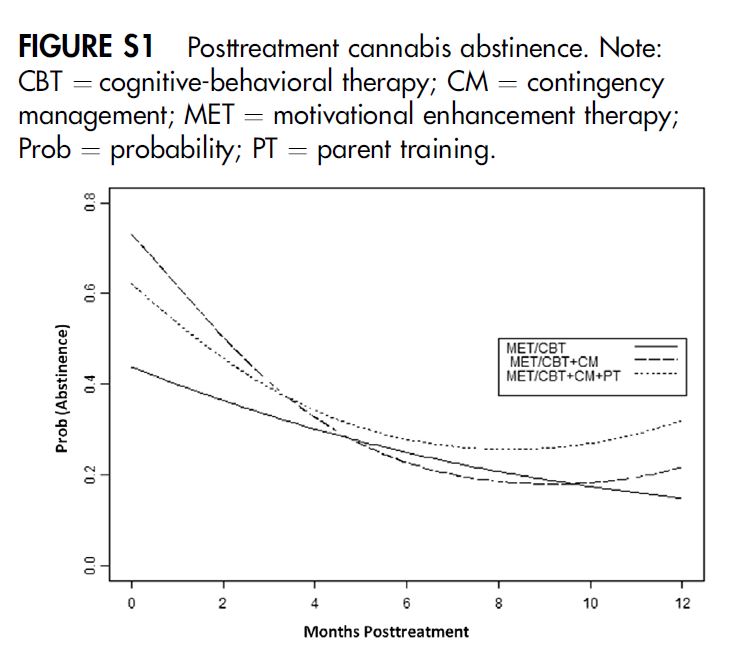
At the end of treatment, MET/CBT+CM (75%) had a higher likelihood of a negative toxicology screen than MET/CBT (41%), while MET/CBT+CM+parent involvement (PT) (63%) were not different from either of the other groups.
However, participation in the weekly continuing care toxicology screens was low (about 3 screens completed out of a possible 12).
Also, across 3-, 6-, 9-, and 12-month follow-up assessments, abstinence rates declined in a similar fashion for all groups, with no group differences at follow-ups (e.g., negative toxicology screen proportions were 41%, 39%, and 41% for MET/CBT, MET/CBT+CM, and MET/CBT+CM+parent involvement (PT), respectively, at 3-month follow-up).
Groups all declined on percent days of cannabis use during treatment, and remained stable during the follow-ups, but were not different from each other. Interestingly, parents’ positive involvement as measured by the Alabama Parenting Questionnaire decreased in MET/CBT+CM+parent involvement (PT) relative to the other two groups, and patients in this group had the highest levels of externalizing problems at the end of treatment.
IN CONTEXT
This methodologically rigorous study showed that adding contingency management in response to toxicology screen results, including office-based rewards and parent-managed, home-based rewards and negative consequences, can improve the effectiveness of MET/CBT for adolescents with cannabis use disorders.
Adding a separate parent skills training to target non-substance use behaviors did not enhance outcomes, and in this study, did not appear to enhance parenting skills either.
Authors speculated that relatively low adherence to the designed parent training, and/or perhaps low potency of the training itself, may have accounted for the absence of benefit. One other hypothesis is that targeting substance use through CM at home required a large proportion of parent time and resources; additional training and targeting of other problem behaviors may have over-burdened parents in this sample, which had a greater proportion of minority and lower socio-economic status (SES) families than in typical studies of adolescent treatment and recovery.
BOTTOM LINE
- For individuals & families seeking recovery: Consider providing rewards and/or negative consequences for negative toxicology screens (abstinence) or positive toxicology screens (drug use), respectively, on a systematic basis. Based on the study, gift cards to a store, dinner at his/her favorite restaurant, gradual rewards toward a video game, and/or use of the car on the weekend may assist recovery.
- For scientists: First, studies to tease apart the relative influence of office and home-based CM could inform treatment recommendations, particularly as related to parent involvement in their child’s treatment. Second, as in other studies of contingency management, treatment benefit decays once the rewards/consequences are no longer provided. Although researchers attempted to add a continuing care phase, participation was low. More innovative ways to engage adolescents and their families in continuing care may be needed (see here and here for examples). Third, studies that examine neurobiological and other mechanisms of treatment and recovery, in context of methodologically rigorous tests of psychosocial treatments as in the current study, could enhance adolescent treatment and recovery approaches.
- For policy makers: Contingency management is among the most evidence-based approaches to treat substance use disorder (SUD). Consider policies that offer funding to enable treatment centers to provide rewards for negative toxicology screens and/or work with parents to do so over the long-term as short term results decay quickly.
- For treatment professionals and treatment systems: If you have the resources, contingency management interventions and/or training parents to implement contingency management at home are likely to improve outcomes for your adolescent patients with marijuana use disorders. These are powerful interventions while they are in place. The key to longer term success may be being able to apply contingent reinforcement for at least a year to facilitate brain changes or lifestyle changes that are conducive to long-term remission and recovery.
CITATIONS
Lee, D. C., Stanger, C., & Budney, A. J. (2015). Lee, D. C., Stanger, C., & Budney, A. J. (2015, February 2). A Comparison of Delay Discounting in Adolescents and Adults in Treatment for Cannabis Use Disorders. Experimental and Clinical Psychopharmacology. Advance online publication. http://dx.doi.org/10.1037/a0038792

