Does Incorporating Mindfulness Into Relapse Prevention Improve Long-term Substance Use Outcomes?
There is an increasing body of literature suggesting that mindfulness training may be efficacious in treatment of substance use disorders.
Mindfulness training teaches patients to respond to difficult affective and cognitive states on a moment-by-moment basis in a nonreactive, nonjudgmental way that encourages adaptive coping and self-awareness.
Bowen and colleagues set out to conduct the first randomized, controlled trial which would allow for a scientifically-sound comparison between mindfulness-based relapse prevention, cognitive-behavioral relapse prevention or treatment as usual.
The mindfulness-based relapse prevention intervention consisted of 8 weekly, 2-hour group sessions with 2 therapists. The first few sessions provided patients with a foundation in mindfulness and subsequent sessions focused on mindfulness practices, self-care and social support. The cognitive-behavioral relapse prevention intervention was similar to the mindfulness-based program with respect to treatment dose, environment and expectations (e.g. amount of homework).
Topics included:
- assessing high-risk situations
- coping skills
- problem solving
- goal-setting
The treatment as usual condition was a 12-step abstinence-based open-formal group treatment that consisted primarily of discussions. These groups were held 1-2 times per week for 1.5 hours.
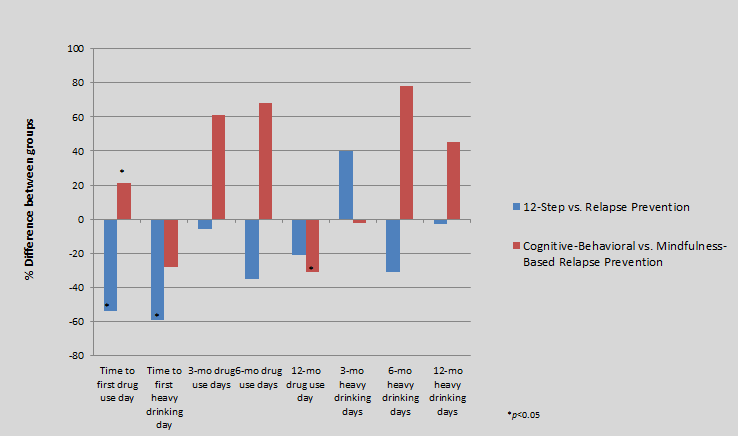
To assess the relative efficacy of mindfulness-based relapse prevention, the researchers compared time to relapse (drug use or heavy drinking) between groups over 1 year. Compared to the 12-step abstinence-based group, the mindfulness and cognitive-behavioral relapse prevention groups showed a 54-59% decreased risk of relapse.
Key Findings Included:
- The mindfulness-based relapse prevention program was associated with increased relapse risk to first drug use, when compared to the cognitive-behavioral relapse prevention program
- There was not a significant difference between the two relapse prevention groups with respect to time to relapse for heavy drinking
- There were no significant group differences with respect to drug use days, any drug use, heavy drinking days or any heavy drinking at the 3-month follow-up.
- At the 6-month follow-up, the two relapse prevention group members who reported any heavy drinking had 31% fewer days of heavy drinking compared to the 12-step abstinence-based group
- The relapse prevention groups had higher probability of abstinence from drugs and heavy drinking.
- There were no significant differences between the two relapse prevention groups
- At 1-year, participants in the mindfulness-based relapse prevention group were less likely to report heavy drinking and reported 31% fewer drug use days as compared to the cognitive-behavioral relapse prevention group
IN CONTEXT
The cognitive-behavioral relapse prevention group was most efficacious in extending time to relapse post-treatment. Both the cognitive-behavioral and the mindfulness-based relapse prevention group showed greater odds of reducing relapse risk as compared to the 12-step abstinence-based group treatment. As time progressed, the treatment condition did not appear to be important in terms of substance use outcomes (6 months) until the 1-year mark at which point the mindfulness-based relapse prevention group appeared to be the most efficacious at reducing drug use and heavy drinking. When considered together, this research suggests that relapse prevention groups are efficacious in reducing relapse risk, however the relative benefits may differ in the short- vs. long-term.
Cognitive-behavioral relapse prevention seemed to have the greatest benefit shortly after treatment, whereas mindfulness-based relapse prevention extended the benefits and reduced relapse risk in the long-term.