Does Race Impact the Effect of Treatment on Future Criminal Activity?
While the quality of care for substance use disorders (SUDs) is improving through the addition of evidence-based treatments and program evaluation, certain racial/ethnic groups may not benefit from these advances due to treatment disparities.
According to the Institute of Medicine (IOM), health disparities are defined as “racial or ethnic differences in the quality of health care that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention.”
Such disparities have been observed for general medical care, but little is known about disparities in SUD treatment.
Acevedo and colleagues examined disparities in the probability of treatment engagement and then looked for differences in the association between treatment engagement and reduced likelihood of arrest by racial group. Institute of Medicine criteria were used to create the following racial categories: Latino (Hispanic/Latin origin, regardless of race), non-Hispanic White, non-Hispanic Black, non-Hispanic American Indian, and other (all other groups and those who are of more than one race).
For this study, treatment engagement was observed only in outpatient settings, and defined with a two-step process: treatment initiation referred to receiving treatment within 14 days of diagnosis (i.e., intake evaluation), and among those who initiate treatment, engagement referred to having two or more additional services within 30 days of initiation. The study population consisted of adult clients who began new outpatient substance use disorder (SUD) treatment (never having received treatment, or not having received treatment for at least 60 days) in 2008 in Connecticut (n = 5,666), New York (n = 86,476), Oklahoma (n = 8,105), and Washington state (n = 8,407).
There was wide variation in racial makeup of patients by state. Oklahoma and Washington had the largest percentage of American Indians (14% and 12%, respectively), New York had the largest percentage of Blacks (about 30%), and Connecticut and New York had the largest percentage of Latinos (22% and 19%, respectively). Half of the patients in Connecticut, Oklahoma, and Washington had an arrest or incarceration in the year prior to outpatient treatment, compared to only 18% in New York.
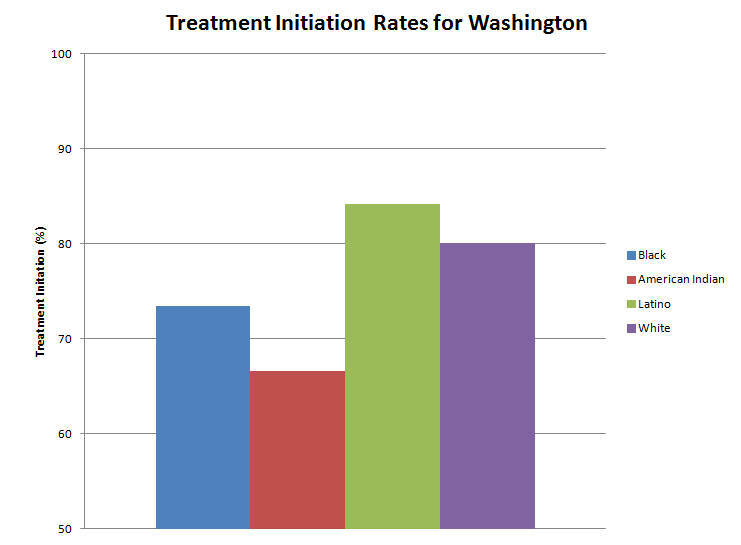
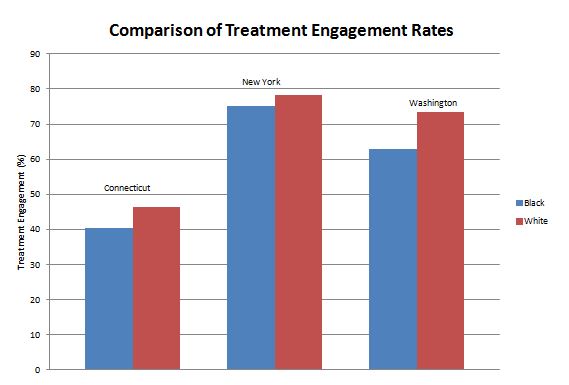
When looking at arrests in the year following treatment, for each racial group in New York, patients who engaged in treatment had lower arrest rates than those who did not, as did Blacks and Whites in Oklahoma, and Whites and Latinos in Washington. When adjusting for socioeconomic variables such as education, employment status, and homelessness, the authors reported the following significant results: Latinos (vs. Whites) were more likely and Black patients (vs. Whites) less likely to engage in care in New York, and American Indians (vs. Whites) were less likely to initiate and engage in treatment in Washington.
The authors also used longitudinal methods to examine time to arrest after outpatient treatment initiation. The likelihood of arrest was higher for Blacks than Whites in Connecticut, New York, and Washington (Hazard Ratio [HR]: 1.3, 1.16, and 1.44, respectively). This means, for example, that the likelihood of arrest was 30% higher for Blacks compared to Whites in Connecticut.
The likelihood of arrest was lower for patients in New York, Oklahoma, and Washington (HR: 0.64, 0.78, and 0.81, respectively), meaning that patients engaged in treatment in New York were 36% less likely to be arrested than patients who were not engaged in care. In New York, Blacks and Latinos (vs. Whites) had significantly muted effects of engagement on reduced likelihood of arrest compared to Whites (HR: 1.29 and 1.33, respectively). In Washington, American Indians (vs. Whites) had significantly reduced effects of engagement on reduced likelihood of arrest (HR: 1.37).
This is an important finding clinically as the longer lag between index visit (e.g. evaluation) and treatment initiation predicted a lower likelihood of treatment engagement in all states irrespective of racial grouping. In this methodologically sound, and clinically informative study, authors showed that certain ethnic groups are less likely to engage in (particularly Blacks in comparison to Whites) and to benefit from substance use disorder (SUD) treatment in terms of reduced later likelihood of arrest (for Blacks and Latinos compared to Whites).
IN CONTEXT
After identifying substance use disorder (SUD) treatment disparities for racial/ethnic groups, a crucial next step is to address the causes of these gaps in care. The cultural aspects related to care should be addressed in a sensitive manner to ensure that minority patients feel comfortable seeking help and returning for care once treatment is initiated.
For people who are arrested for non-violent drug crimes, supportive services such as linkage to substance use disorder (SUD) treatment may be more beneficial than punishment under the existing minimum sentencing laws.
- LIMITATIONS
-
When associating engagement in care with criminal justice outcomes such as arrest, it is important to recognize structural and societal factors that may bias these results. For example, Blacks are arrested for drug possession at a rate three times that of Whites despite comparable levels of illegal drug use, suggesting other factors are at play. Additionally, Blacks comprise over 60% of the prison population though they represent only 30% of the U.S. population.
NEXT STEPS
Future studies should examine what community-level factors influence treatment seeking behavior for different racial groups as well as evaluating the quality of services offered in these areas.
BOTTOM LINE
- For individuals & families seeking recovery: Minorities in need of substance use disorder (SUD) treatment, it is important to try to verbalize any concerns with your treatment provider if you feel your needs are not being adequately addressed. The sooner treatment is initiated after initial evaluation, the more likely is is to see full engagement in treatment.
- For scientists: More studies are needed to examine barriers related to SUD treatment for minority groups. Studies looking at effectiveness of interventions should also focus on minority groups as the target population; results from studies where a majority of participants are White may not be generalizable to different ethnic groups.
- For policy makers: Structural barriers that prevent equality in SUD treatment by ethnic/racial groups should be identified and addressed. A shift towards treatment in the criminal justice system is also needed as drug offenders have a re–arrest rate of approximately 66% and about 70% of state and 64% of federal prisoners regularly used drugs before they were incarcerated (see here).
- For treatment professionals and treatment systems: This study emphasizes the importance of cultural sensitivity towards the populations you are serving. Being cultural sensitive may help retain minority patients in care.
CITATIONS
Acevedo, A., Garnick, D. W., Dunigan, R., Horgan, C. M., Ritter, G. A., Lee, M. T., … & Leeper, T. (2015). Performance measures and racial/ethnic disparities in the treatment of substance use disorders. Journal of studies on alcohol and drugs, 76(1), 57-67.

