The economic impact of recovery management checkups
Recovery Management Checkups are a long-term clinical approach to following up with patients with substance use disorder much like treating other chronic illnesses like hypertension or diabetes. Prior research has shown that this approach, which includes quarterly checkups, helps enhance long-term recovery outcomes. Can investment in this approach ultimately save health care costs?
Like many other treatments, given the additional money needed to implement these checkups, understanding its overall economic impact is key.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Severe substance use disorders are treatable chronic health conditions often characterized by a course of alternating periods of remission and relapse before long-term sustained remission is achieved. As a result, Recovery Management Checkups were designed to respond to the chronic nature of the recovery process by checking-in with patients on a quarterly basis, and providing an active linkage back to treatment for those who need it.
This early re-intervention can help to prevent relapse or intervene early before it becomes severe. Rigorous studies have shown Recovery Management Checkups help improve long-term substance use outcomes compared to simply monitoring individuals over time. The economic impact of this intervention, however, is unknown.
Given that policy makers and other stakeholders often want to know whether the additional costs of providing recovery management checkups are worth the benefits in terms of improved substance use outcomes and other associated benefits (e.g., health, criminal justice, and workplace issues), this study fills an important gap in the literature.
HOW WAS THIS STUDY CONDUCTED?
This study is an analysis of a randomized clinical trial of outcome monitoring alone (control condition which received quarterly assessments only) compared to Recovery Management Checkups + outcome monitoring (experimental condition). Participants in the experimental condition who were identified as ‘in need’ during a quarterly assessment were connected to linkage managers. ‘In need’ was identified by problematic substance use without current treatment. Linkage managers performed a number of activities including accompanying participants through intake and scheduling appointments, all intended to help them fully re-engage with the treatment system.
The clinical trial was conducted at the largest central intake unit for substance use disorders in Chicago, Illinois in the year 2004. Participants include 446 patients who were 38 years old on average, 54% male, mostly African American (85%), most had experienced homelessness at least once (62%), and most were currently unemployed (68%). Data on the quarterly cost per participant came from previous studies of intervention costs and effectiveness dataresults are presented for incremental cost, incremental effectiveness and the incremental cost-effectiveness ratio for two outcomes: abstinence and substance use-related problems. Incremental cost-effectiveness is the cost of achieving one more day of abstinence or one fewer substance use-related problem for participants in the Recovery Management Checkup group versus outcome monitoring group. Substance use-related problems were considered to be 16 potential symptoms (e.g., complaints about use, hiding use, DSM-IV dependence or abuse symptoms, or health or mental health problems related to substance use).
An analysis was conducted to test the consistency of the results from the cost-effectiveness analysis (known as a “sensitivity” analysis). By adding in the cost of other areas such as health services, social services, criminal justice, and employment problems, the authors could see if the results of the cost-effectiveness analysis changed. Financial conversions came from many data sources such as the American Medical Association, Agency for Healthcare Research and Quality, and others.
WHAT DID THIS STUDY FIND?
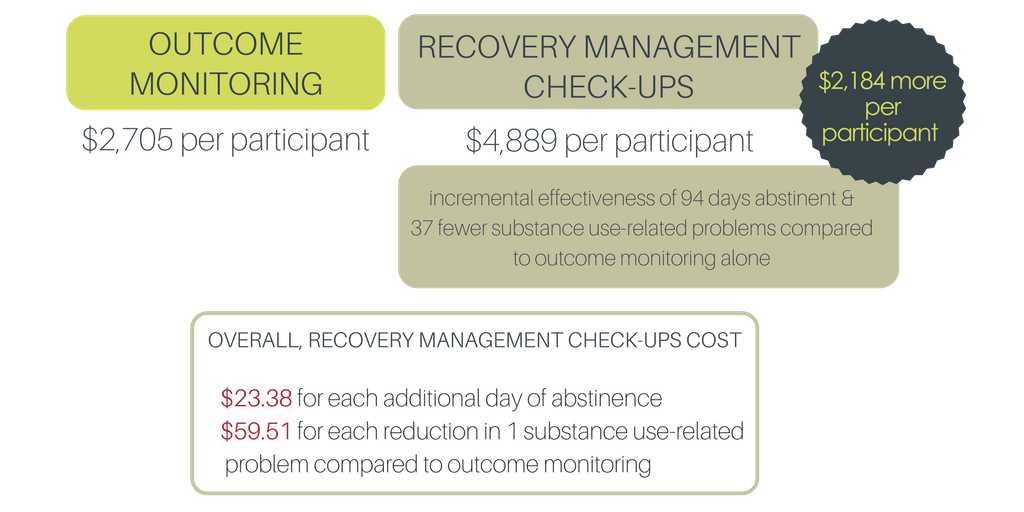
Over a four year period, Recovery Management Checkups cost $2,184 more per participant compared to outcome monitoring (i.e., $4,889 for Recovery Management Checkups – $2,705 for outcome monitoring = $2,184). Recovery Management Checkups had an additional incremental effectiveness of 94 days abstinent and 37 fewer substance use-related problems compared to outcome monitoring alone. Overall, Recovery Management Checkups cost $23.38 for each additional day of abstinence and $59.51 for each reduction in one substance use-related problem compared to outcome monitoring
An additional analysis was run (i.e., cost-effectiveness acceptability curve) to estimate the cost to society if they wanted a nearly 100% chance that the intervention is cost-effective compared to outpatient monitoring alone. The results indicated that if society paid $60 per day of abstinence, the probability that the intervention is cost-effective approaches 100%. If society paid $100 for each one unit reduction in substance problem, the intervention has a greater than 90% chance of being cost-effective.
When considering other societal costs associated with substance use – that were directly measured by the study – Recovery Management Checkups had costs equal to or lower than monitoring alone. Specifically, Recovery Management Checkups generated fewer costs to society over four years ($21,763) than outcome monitoring alone ($24,048). When societal costs were combined with intervention costs, the total intervention cost became $26,652 for Recovery Management Checkups and $26,750 for outcome monitoring. Given that Recovery Management Checkups had better outcomes at similar costs, when other societal outcomes are considered, Recovery Management Checkups dominate monitoring in terms of cost-effectiveness.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This is the first economic evaluation of Recovery Management Checkups for long-term outcomes (i.e., four years) from substance use disorder treatment.
Quarterly Recovery Management Checkups appear to be a cost-effective strategy for promoting recovery compared to outcome monitoring alone.
The full economic impact was approximately equal between the two conditions; however, participants who received Recovery Management Checkup still had significantly more days of abstinence and fewer substance use-related problems than those receiving outcome monitoring only.
This type of approach could be applicable in any setting where individuals are worried about the perceptions of seeking help for an alcohol and other drug problems, such as in health care settings, for the staff themselves.
- LIMITATIONS
-
- The results of this study are based off a single trial in an urban African American population thus generalizability to other geodemographic populations is not currently known. It could be more or less cost-effective in other populations.
NEXT STEPS
The authors have suggested that in order to compare Recovery Management Checkups in terms of cost-effectiveness to other treatable chronic conditions (e.g., diabetes, hypertension), estimates of length of time lived at varying levels of health (i.e., quality-adjusted life years) or perhaps life expectancy would be required.
BOTTOM LINE
- For Individuals and families seeking recovery: Cost-effectiveness studies are a form of economic analysis designed to compare the relative costs and outcomes of different courses of action. In this case, Recovery Management Checkups (which actively links people back to the treatment system when they need it over time) were compared to outcome monitoring alone without the checkup or linkage. Over four years, Recovery Management Checkups were delivered quarterly and produced 94 more days of additional abstinence and 37 fewer substance use problems. When all costs were considered, the costs were about the same and the substance use outcomes were better. Long-term clinical management of substance use disorder is not only an effective strategy to help your loved one get and stay in recovery but also appears to be a cost-effective health care service.
- For scientists: This study found that Recovery Management Checkups are more cost-effective than outcome monitoring alone. Next steps may be to compare who in particular may need and benefit from this type of service and to investigate how the positive effects might be amplified. In addition, further comparative effectiveness studies with other diverse samples are needed to establish its potential benefits more definitively.
- For policy makers: This study conducted a four year follow-up to determine the cost-effectiveness of Recovery Management Checkups compared to outcome monitoring alone. The full economic impact was approximately equal between the two conditions after incorporating the societal costs (health services, social services, criminal justice, and employment); however, participants who received Recovery Management Checkups still had significantly more days of abstinence (94 days) and fewer substance use-related problems (37 fewer problems) than participants who received outcome monitoring only. Recovery Management Checkups were thus superior in terms of cost-effectiveness.
- For treatment professionals and treatment systems: In this well-designed study, the authors conducted a four year follow-up of an experimental investigation designed to test the effects of Recovery Management Checkups to outcome monitoring. Recovery Management Checkups appear to be more cost-effective in terms of its ability to increase abstinence and decrease substance-problems. The average cost per day ($23.38 versus $59.51) are low considering this intervention targeted a high-cost disadvantaged population in the current study.
CITATIONS
McCollister, K. E., French, M. T., Freitas, D. M., Dennis, M. L., Scott, C. K., & Rodney, R. F. (2013). Cost-effectiveness analysis of recovery management checkups (RMC) for adults with chronic substance use disorders: evidence from a 4-year randomized trial. Addiction, 108, 2166-2174.

