Integrating Substance Use Disorder Treatment & Primary Health Care
Approaches that integrate addiction treatment with primary health care are needed now more than ever because: 1) we understand substance use disorder to be a chronic illness requiring ongoing recovery management rather than isolated episodes of treatment & 2) there has been a shift in health care to emphasize both effectiveness and lower costs
Can an intervention linking individuals in substance use disorder treatment to primary health care enhance both patient health care engagement and abstinence?
WHAT PROBLEM DOES THIS STUDY ADDRESS?
If substance use disorders are to be treated as chronic diseases, as many experts have suggested, primary care will likely have to play a significant role. Primary care doctors already have ongoing, long-term follow-ups with their patients, and are well trained to make referrals to specialty treatment when it is needed.
Recently, accessibility to one’s primary care doctor has increased with the introduction of electronic documentation (e.g., health records) & communication (e-mail) platforms.
This technology increases the potential positive role primary care could play in helping individuals with substance use disorder manage their recoveries over time, particularly after they complete what are often short (2-6 week) episodes of addiction treatment.
How well patients are equipped to take an active role in their addiction related care, and to use the primary care services available to them, are unclear. This is often referred to as “patient activation”, which is more specifically defined as “understanding one’s role in the care process and having the knowledge, skill, and confidence to manage one’s health and health care.”
This study by Weisner and colleagues tested whether a treatment designed specifically to increase patient activation, improved substance use and mental health outcomes for individuals in addiction treatment.
HOW WAS THIS STUDY CONDUCTED?
The patient activation intervention, called LINKAGE, consisted of groups two times per week for 3 weeks, for a possible total of six groups and was integrated into an existing 6-week outpatient substance use disorder (SUD) treatment. LINKAGE was compared to the usual medical education group that was already standard in the 6-week SUD treatment.
LINKAGE consisted of:
- education on how health care engagement is related to overall well being
- how to engage with the health care system
- strategies to enhance communication with doctors
- strategies to increase electronic documentation access and communicate with doctors (e.g., laboratory results, e-mail, and educational pamphlets)
The intervention also allowed patients to ask for their therapists’ help in communicating with the primary care physician as needed. Patients were assigned to either LINKAGE or the usual medical education depending on when they entered treatment in 3-month segments, whereby the LINKAGE intervention was included in the substance use disorder (SUD) treatment then subsequently withdrawn (an “on/off” design).
The standard outpatient addiction treatment that all patients received involved:
- two daily groups
- individual therapy
- 12-step meetings
- weekly toxicology screens and breathalyzer assessments
The 252 individuals receiving LINKAGE and 251 individuals receiving usual medication education were compared on:
- how well they were retained in substance use disorder (SUD) treatment
- alcohol and other drug abstinence and heavy drinking
- depression (measured by the 9-item patient health questionnaire)
- health care behaviors thought to increase substance use and mental health outcomes, including:
- patient activation (measured by a 13-item scale)
- patient log-in days to the online portal giving them access to certain parts of their electronic medical record
- use of this patient portal (e.g., e-mailing doctors, accessing test results, and obtaining educational information or medical advice)
- communication with primary care physician about alcohol and other drug problems (yes/no)
- PARTICIPANT DEMOGRAPHICS
-
- Despite not being randomized, the sequential on/off study design led to roughly equivalent groups in terms of their demographic and clinical characteristics when they began treatment.
- The sample was primarily 31-45 (39-42%) or 46-60 (34%) years old, with a smaller proportion of 18-30 year olds (16-22%), and 61+ year olds (4-10%).
- They were mostly male (70%) and White (60%), though minority representation – 20% Hispanic, 7-8% Black, and 6-7% Asian – was good compared to other studies.
- There was also a mix in terms of level of education (with high school graduates or less, some college, and college degrees or higher all well represented) and household income (half had household incomes above 50,000).
- Most had access to a computer or smartphone (91%) and could receive e-mail (92%), which is relevant because the intervention encouraged individuals to access their online patient portal, which required internet access.
- Alcohol use disorder was the most common type of substance use disorder (65%) in the sample, followed by opioid (17%), cocaine (16%), and marijuana (12%).
WHAT DID THIS STUDY FIND?
There were no statistically significant differences between the groups 6 months after they entered the study (4.5 months after they completed treatment) on their substance use disorder treatment attendance (79 days for LINKAGE vs. 71 days for usual medication education), abstinence rates (71 vs. 67%), heavy drinking in the past 30 days (13 vs. 19%), or in the proportion of the group with moderate to severe depression defined as a depression score 15 or higher (8 vs. 7%), or with psychiatric disorder in addition to substance use disorder.
However, those who received all six sessions (compared to five or fewer) as well as those who used the option of having their therapist help with physician communication did have better treatment attendance, as well as a greater percentage of individuals with alcohol abstinence and lower percentage of individuals with heavy drinking.
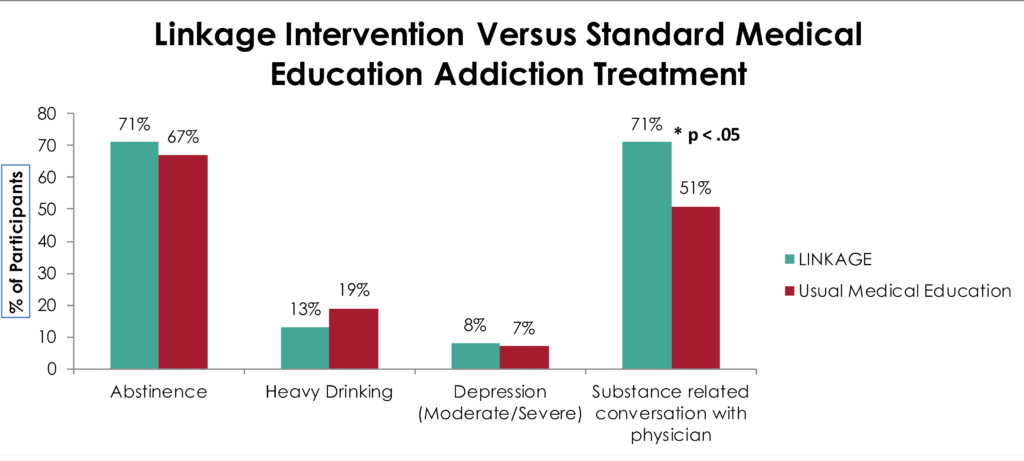
Despite these similar substance use and mental health outcomes, LINKAGE patients were more engaged health care participants. They had twice as many log-in days to their patient portal during the intervention, an advantage maintained through the 6-month follow-up, and were also more likely to talk with their primary care physician about their alcohol and drug use at 6-month follow-up (71 vs. 51%).
While more of the LINKAGE patients with a co-occurring psychiatric disorder, such as major depressive disorder, had a meaningful increase in their patient engagement at the 6-month follow-up (3 or more points; 61 vs. 51%), this did not quite reach the threshold considered to be statistically reliable.
WHY IS THIS STUDY IMPORTANT?
This study was an important step in our efforts to bridge specialty substance use disorder (SUD) treatment and primary health care.
Although LINKAGE may help enhance patient engagement in primary care, it did not impact their ultimate outcomes out to 6 months.
As authors point out, it may take several more months (or years) to observe benefits of better engaging addiction treatment patients to primary health care. While there were better outcomes for individuals who attended all six LINKAGE sessions or for those who used the therapist facilitated health communication option, this could also reflect more motivation and eagerness to get well in this group.
Another study that attempted to improve health care engagement among individuals with substance use disorders (SUD) had similar types of results. The AHEAD trial tested chronic care management (CCM) to engage alcohol/drug addicted individuals with addiction treatment resources. Despite the chronic care management group’s increased addiction treatment utilization, they were not different on substance use outcomes compared to usual primary care, which included providing patients with a list of treatment resources despite increased addiction treatment utilization.
This lack of effectiveness was also true for those who had co-occurring psychiatric disorders in addition to substance use disorder, a study we reviewed in a previous Recovery Bulletin. One major difference between that study and the current study is that in LINKAGE, the intervention was delivered in specialty substance use disorder treatment and intended to engage individuals with primary care, while AHEAD was delivered in primary care and intended to engage individuals with substance use disorder treatment services.
Efforts to integrate substance use disorder (SUD) treatment and primary care lead to more overall health care engagement, but not better substance use or mental health outcomes.
- LIMITATIONS
-
- This study had a strong design overall. Although patients were not randomized to the intervention – often considered the gold standard of establishing the intervention caused the outcome – an on/off design is considered the best alternative when two or more interventions are being tested against each other within the same clinical program or setting.
NEXT STEPS
The most important next step seems to be more extensive intervention or perhaps a different approach. Also, longer-term follow-up might be needed as 6 months may not be a sufficient amount of time to capture LINKAGE’s benefit. . One piece of that long-term follow-up would ideally include how quickly individuals are able to re-initiate abstinence or low-risk drinking with or without specialty care after relapse.
An intervention protocol known as “recovery management checkups”, for example, that checks in with patients following substance use disorder (SUD) treatment every 3 months over several years, has been shown as a cost-effective approach that gets people back into treatment sooner when they need it and improves outcomes over time.
BOTTOM LINE
- For individuals & families seeking recovery: There are ways to help someone with substance use disorder to make the most out of the health care offered to them, and to effectively communicate with their primary care doctor. This intervention could have an influence on their long-term outcomes but more research is needed to say this definitively.
- For Scientists: This methodologically rigorous trial found that LINKAGE, a treatment designed to engage substance use disorder treatment patients with primary care, enhanced proximal (primary care engagement) but not distal outcomes (substance use and depression). Long-term studies may be needed to help determine whether this better engagement could lead to better outcomes down the road for these individuals.
- For Policy makers: In the age of accountable care organizations and overall emphasis on cost-effective recovery management options for individuals with substance use disorder, developing and evaluating treatments that integrate specialty addiction treatment with primary care are very much needed. This study suggests one such treatment, LINKAGE, may be a promising option, though longer-term studies are needed. Allocating funding to studies such as these could yield information that would help answer the question of best practices in the emerging health care system.
- For Treatment professionals and treatment systems: LINKAGE is a treatment designed to be added to outpatient substance use disorder treatment that more effectively engages substance use disorder treatment patients with primary care. This study suggests LINKAGE type procedures may be useful but more research is needed to understand how greater healthcare engagement may enhance SUD outcomes.
CITATIONS
Weisner, C. M., Chi, F. W., Lu, Y., Ross, T. B., Wood, S. B., Hinman, A., . . . Sterling, S. A. (2016). Examination of the Effects of an Intervention Aiming to Link Patients Receiving Addiction Treatment With Health Care: The LINKAGE Clinical Trial. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2016.0970

