Kratom: What is it, who’s using it, and why?
Kratom, a plant native to Asian countries, was recently introduced to the United States and is growing in popularity. Although not approved by the FDA for substance use disorder treatment, this study suggests that about one-quarter of addiction treatment patients have used kratom, and the majority of them are using it to self-treat opioid use disorder symptoms.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Individuals in Asian countries have used the kratom plant for medical and recreational purposes for centuries. Often taken orally, kratom can produce stimulant-like effects or pain-relieving and anti-anxiety effects depending on the strain of the plant and the dose that is taken. Kratom has been associated with a variety of benefits (e.g., pain relief, mood enhancement, increased energy). This is because two compounds in kratom leaves (mitragynine and 7-α-hydroxymitragynine) interact with opioid receptors in the brain, producing sedation, pleasure, and decreased pain, especially when users consume large amounts. Potential side effects include dry mouth, fatigue, and seizure. Randomized controlled trials have not yet been conducted and kratom’s effects on the brain and behavior appear to be unlike those of more common drugs like marijuana, opioids, and stimulants. Kratom’s availability has recently increased in non-Asian countries like the U.S., and reports suggest that individuals may be using Kratom to substitute drug use, ease withdrawal, and alleviate physiological drug dependence, including opioid dependence. However, it is unclear how common kratom use is for these purposes, as kratom may have the potential to induce dependence-like symptoms (withdrawal and craving). The current study aimed to address this gap by examining the prevalence of, and motivations for, kratom use among individuals receiving substance use disorder treatment.
HOW WAS THIS STUDY CONDUCTED?
The authors administered a 49-item questionnaire to 500 substance use disorder patients (58% male; average age of 35 years) attending one of five 12-step-based, residential therapeutic community programs. Participants were asked about demographics, health information, lifetime and past-year substance use, focusing specifically on kratom use. The authors sought to characterize lifetime and past-year kratom use prevalence, motivations for kratom use, and its perceived benefits/side-effects. They also compared individuals with a history of kratom use to those without a history of kratom use on demographics, treatment and emergency department service use, and substance use histories.

Figure 1. Depicts the kratom leaf and its appearance when ground into a fine powder for ingestion.
WHAT DID THIS STUDY FIND?
Kratom use prevalence.
- 21% of patients reported lifetime kratom use and 10% reported kratom use in the past year.
Demographics and service use.
- Compared to those who had not used kratom, individuals with lifetime kratom use:
- Were younger and more educated.
- Were younger (average age = 32 vs. 36 years), and more likely to have an associate’s or bachelor’s degree (24% vs. 12%).
- Had higher rates of homelessness and more extensive treatment and emergency service use histories.
- Were more likely to have experienced past-year homelessness (10% vs. 4%), to report previous receipt of addiction treatment (83% vs. 64%) and past-year emergency room utilization for drug-related (61% vs. 38%), mental health-related (41% vs. 19%), and physical health-related (68% vs. 52%) reasons.
- Reported a greater number of previous substance use interventions (4 vs. 3) and a greater number of months spent in other treatment programs (1.8 vs. 1.2 months) in the past year.
- Had more extensive incarceration histories.
- Were less likely to be on probation/parole at the time of the survey (69% vs. 83%) but had been incarcerated a greater number of times (7 vs. 5).
- Had similar rates of chronic pain, disability, medical insurance, employment, and race.
- Were younger and more educated.
Substance use histories.
- Individuals who had used kratom had more extensive substance use histories than those who had not used kratom. Almost all substances were more prominently used in the kratom group across the lifetime (except alcohol and marijuana) and in the past year (except alcohol and barbiturates).
- None of the participants reported kratom as a drug of choice. Among individuals who had a lifetime history of kratom use and no history of kratom use, opioids and amphetamines were the most commonly reported drugs of choice. Notably, compared to those with no history of kratom use, individuals with a history of kratom use were more likely to report heroin (50% of individuals with kratom use history vs. 30% of individuals with no kratom use history) and Suboxone (5% of individuals with kratom use history vs. 3% of individuals with no kratom use history) as a drug of choice.
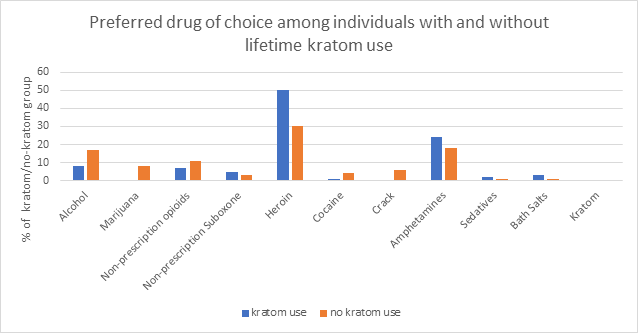
Figure 2.
Kratom use motivations and perceived benefits.
- Common reasons for using kratom included 1) using to reduce or stop opioid use (60%), 2) using to cut back or get off of opioids (69%), and 3) using it as an opioid substitute (64%).
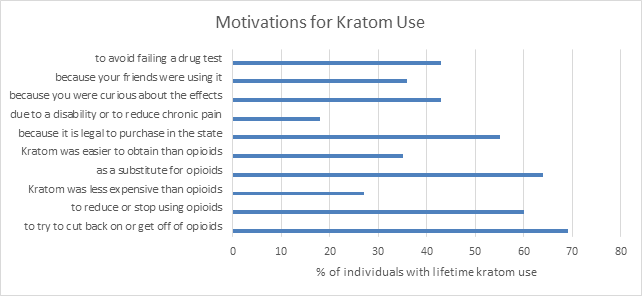
Figure 3.
- 33% said they would try kratom again and 31% thought kratom was a helpful drug. 27% said kratom had fewer unpleasant side effects than opioids and <10% reported negative side effects from using kratom. <10% reported preferring the high of kratom use to the high of opioid use.
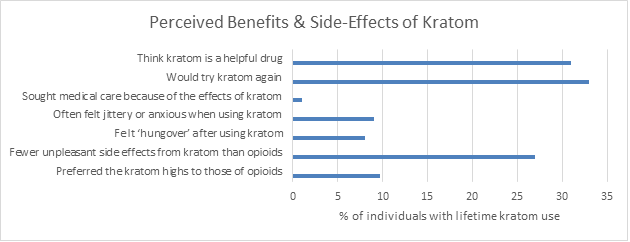
Figure 4.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study suggests that about one-quarter of this treatment-seeking population has used kratom (10% had past year use). Its use as an opioid substitute was rather common, with just under 70% reporting kratom use to help cut back or quit opioid use. Furthermore, less than 10% reported negative mental or physical side effects from kratom. Given that kratom does not appear to be a drug of choice and that the majority of patients didn’t prefer its ‘high’ over that of opioids, kratom may have treatment potential for helping individuals alleviate opioid use disorder symptoms. However, kratom has not been studied in randomized controlled trials to-date, so its benefits and risks are not yet fully understood. Although kratom may have the potential to help relieve pain, improve mood, induce relaxation, and enhance socialization and energy, it has also been associated with various side effects, which are likely dependent on dose, strain, and duration of kratom use. These might be some of the reasons why less than one-third of those exposed to the drug in this sample thought it was helpful. Other mild side effects include constipation, dehydration, dry mouth, fatigue/lethargy, increased body temperature, nausea, and weight loss. More serious side effects, such as seizure, coma, overactive thyroid, and liver damage have also been reported. Kratom is a legal substance in most U.S. states, but strain and dose are largely unregulated and there is some concern that kratom products may be “laced” with other compounds (i.e., adulterated) that can lead to serious adverse effects. There were 44 deaths in 2017 related to kratom use, most of which were likely due to adulterated products. At present there is no reliable evidence for the use of kratom in treating opioid use disorder. Some studies have found that its use may have the potential to result in a physiological dependence on kratom. However, findings are mixed with some individuals reporting low craving and others reporting difficulty refraining from kratom use. Controlled trials are needed to gain a better understanding of whether this plant can help patients or if the cost outweighs the benefits. Nonetheless, kratom use appears to exist in treatment-seeking populations, in large part for self-treatment purposes. The outcomes of this study suggest that kratom use may be more prevalent in individuals who have used a wider variety of substances, exhibit more extensive substance use histories, and greater use of addiction treatment and emergency department services. Creating awareness of kratom, the populations that use it, and the reasons behind it might ultimately help inform policy and addiction treatment. Given our limited knowledge of the risks associated with kratom use, individuals may benefit from discussing kratom with their health care providers. Still, this study provides important preliminary insight to kratom use prevalence and motivations for taking it among treatment seekers. Additional research will help us identify whether or not its use as a medication substitute is justified.
- LIMITATIONS
-
- The authors did not assess current ongoing kratom use or the chronicity, dose, and frequency of kratom use. Although not part of a standard toxicology screen, kratom drug tests are available to detect recent kratom use but were not administered in this study. Therefore, it is unclear how often kratom is taken, the dose it is taken at, and for how long individuals use it, or if kratom use is common in patients during treatment. Additional research is needed to characterize these factors and their associated benefits and side-effects.
- Participants were not excluded for comorbid mental/physical health conditions and had a wide variety of preferred/used substances. Therefore, it is unclear whether kratom use would be more prevalent in populations with specific disorder characteristics, such as primary opioid use disorder patients.
- These data were collected via self–report and were not confirmed using patient medical records. Furthermore, the study assessed a residential treatment population and it is not clear if kratom use prevalence and motivations for use found in this study would translate to the broader substance use disorder population.
BOTTOM LINE
- For individuals and families seeking recovery: This study suggests that about one-quarter of residential treatment seekers have ever used kratom and 10% have used it in the last year. A large majority of patients had used kratom for therapeutic reasons, with 70% using it as an opioid substitute. Although less than 10% of patients reported negative side effects from kratom or drug preference for kratom, its benefits and risks are not yet fully understood. Despite kratom’s potential for helping individuals reduce opioid use, it is unclear whether its use can lead to kratom dependence. Additionally, kratom is largely unregulated and it is difficult to know if retail kratom products contain harmful additives that can lead to more serious consequences. Being aware of kratom and its therapeutic potential, while understanding that science has not yet fully characterized it and products are not guaranteed to be free of harmful additives, can help guide individuals and their families to be more informed throughout the treatment and recovery process. Given the limited knowledge of kratom at present, individuals should check with their health care providers prior to taking it. Additional research will help us to better understand kratom’s effects and therapeutic potential.
- For treatment professionals and treatment systems: This study suggests that about one-quarter of residential treatment seekers have ever used kratom (10% reporting past-year kratom use) and 70% of them reported kratom use for therapeutic reasons (as an opioid substitute). Although less than 10% of patients reported negative side effects from kratom or drug preference for kratom, its benefits and risks are not yet fully understood. Kratom may have the potential to help treat opioid use disorder symptoms, but it may also have the potential to lead to kratom dependence. Given that kratom is largely unregulated, kratom products come with the risk of adulteration, which can lead to serious health consequences. Being aware of kratom’s therapeutic potential and the population characteristics associated with its use, while understanding the limits of kratom’s scientific evidence to-date and the possible risks of use, can ultimately help treatment providers better inform their patients. This study suggests that kratom-use populations are younger and more educated, with higher rates of homelessness and more extensive histories of incarceration, substance use, treatment, and emergency service use. Treatment providers can benefit patients by educating them about kratom’s strain– and dose–dependent effects, its risks, and patient-reported subjective benefits. Providers can also educate themselves by checking with their affiliated treatment programs to see if they have any explicit policies or guidelines around kratom use. Given kratom’s unknown potential for physiological dependence, providers may also want to open a dialogue with patients about whether their use constitutes misuse. As kratom research progresses, a clearer understanding of kratom’s effects and therapeutic potential is sure to emerge.
- For scientists: Kratom use has grown in popularity since its introduction to the U.S., and this study suggests that 21% of residential addiction treatment patients have lifetime kratom use and 10% have past-year kratom use. Motivations for use were largely driven by a desire to alleviate opioid use disorder symptoms. Negative physical/mental health consequences were seldom reported and kratom was not a drug of choice. Despite these outcomes, randomized controlled trials are needed to better understand kratom’s effects and their variability according to strain, dose, and individual characteristics. Although it seems kratom is being used for therapeutic purposes, its therapeutic effects have not yet been demonstrated and the potential for kratom dependence is of concern. Importantly, this study did not assess frequency/quantity of use or current use, demanding additional research to characterize typical kratom use patterns. Many individuals seek alternatives to suboxone treatment for opioid use disorder, and kratom’s potential as an opioid substitute warrants further investigation.
- For policy makers: This study suggests that about one-quarter of residential treatment seekers have ever used kratom, with use largely reported for therapeutic reasons to help reduce or stop opioid use. Although less than 10% of patients reported negative side effects from kratom or drug preference for kratom, its benefits and risks are not yet fully understood. Given its potential as an opioid substitute, additional funding is needed to better understand kratom as a therapeutic option. Kratom research may also inform policy, as kratom is legal in most states, illegal in some states, and opposition/support cannot yet be based on scientifically–grounded conclusions given limited research. Importantly, kratom products are currently unregulated. An estimated 44 kratom-related deaths occurred in 2017, most of which are thought to be due to adulterated kratom products. Identifying ways to regulate kratom to ensure minimal harm is essential to prevent future deaths. Given kratom’s relatively common use in treatment–seeking populations and its potential to alleviate opioid use disorder symptoms, kratom research may ultimately help to address the ongoing opioid crisis.
CITATIONS
Smith, K. E., & Lawson, T. (2017). Prevalence and motivations for kratom use in a sample of substance users enrolled in a residential treatment program. Drug and Alcohol Dependence, 180, 340-348. doi: 10.1016/j.drugalcdep.2017.08.034

