Leveraging opportunities to address early substance use for youth in primary care settings
During adolescence, youth often begin to experiment with alcohol or other drugs. Early intervention is key to preventing substance use consequences. Screening, brief intervention, and referral to treatment (SBIRT) is the recommended evidence-based approach to providing early intervention with youth seen in primary care, but this seldom occurs. This study examined youth substance use reported during primary care visits and examined provider perspectives on the feasibility of doing SBIRT in routine practice.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Adolescence is often termed a time of “storm and stress”, where youth are going through many developmental changes and are also more likely to engage in risk behaviors. One such risk behavior is substance use: adolescence is a key time for youth to try drinking alcohol or using other drugs. For most, this experimentation does not result in life-altering harms. For a subset, however, early intervention at this stage can be key to preventing this exploration from reaching the stage of a substance use disorder (SUD). Yet, research has indicated that not all youth receive early intervention at the same rate: there are marked disparities in access to treatment and to follow-up which vary by race, ethnicity, gender, and other youth characteristics.
Although screening, brief intervention, and referral to treatment (SBIRT; pronounced “essburt”) is the recommended evidence-based approach to intervening with youth when being seen by their doctor for a primary care visit, there is evidence indicating that this does not happen as often as it could in practice. Providers report barriers to even initiating the full SBIRT approach beginning with screening, such as lack of time during clinic visits, or describing a lack of experience with screening or referral to treatment.
To address these gaps and inform SBIRT implementation strategies, the researchers in this study used a multi-method research study approach. They examined the level of self-reported substance use among youth during their primary care visits to a federally-funded health center and whether substance use varied by youth characteristics. They also collected provider perspectives on the feasibility of using SBIRT in their day-to-day practice. Ultimately, the researchers were seeking to inform approaches that would reduce disparities in SUD treatment access among minority adolescents.
HOW WAS THIS STUDY CONDUCTED?
This study used a descriptive, multi-method research approach. The researchers collected data from both youth and providers. Data for the youth sample was from taken from the electronic medical record of youth ages 12-19 years who completed a pediatric primary care well-child visit at a Federally Qualified Health Center between 2014-2017 (N = 2252). Federally qualified health centers are community-based organizations that offer comprehensive health services to patients. They offer services regardless of health insurance status and so they provide primary care and preventive services to publicly insured or underinsured adolescents.
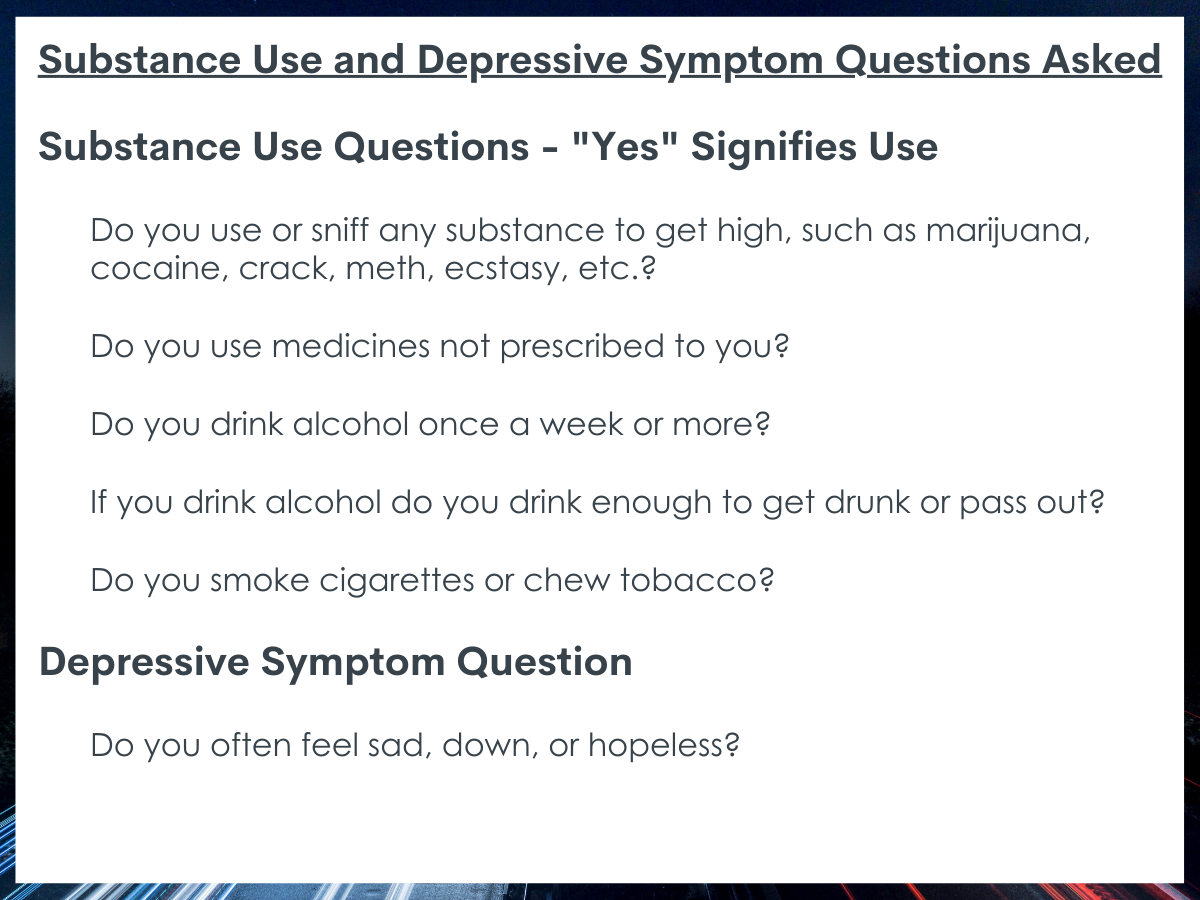
The data used was from the Staying Healthy Assessment, a health assessment tool mandated by Medicaid for clinical centers to complete. Notably, the Staying Healthy Assessment is geared toward assessing current behaviors and not history of those behaviors. Of those 2252 youth with well-child visits, 1588 youth had the Staying Healthy Assessment completed in their electronic medical record and of these around 90% had answered the substance use questions. For the youth with substance use questions answered, the researchers collected demographic characteristics from their record. The researchers also collected data from 12 pediatric care providers using a semi-structured interview guide. The interview guide included questions for providers to (1) describe existing procedures for identifying/addressing youth use, (2) describe their own perceptions and attitudes toward youth substance use, (3) identify barriers to implementing SBIRT, and (4) suggest strategies to address these barriers.
Of the analytic sample of 1436 adolescents who completed the Staying Healthy Assessment and answered the substance use questions, about 67% identified as Hispanic, 10% as non-Hispanic Black, 21% as non-Hispanic Other, and 3% as non-Hispanic White. Around 50% of youth were female, the average age was 14.4 years, and 16% reported experiencing depressive symptoms. The provider participants were in pediatric primary care (n = 7) and urgent care (n = 4) and included 8 physicians and three nurse practitioners. There was also one behavioral health clinician who was a licensed clinical social worker. The majority of provider participants were female (83%) and had been in their role between 4 and 11 years.
WHAT DID THIS STUDY FIND?
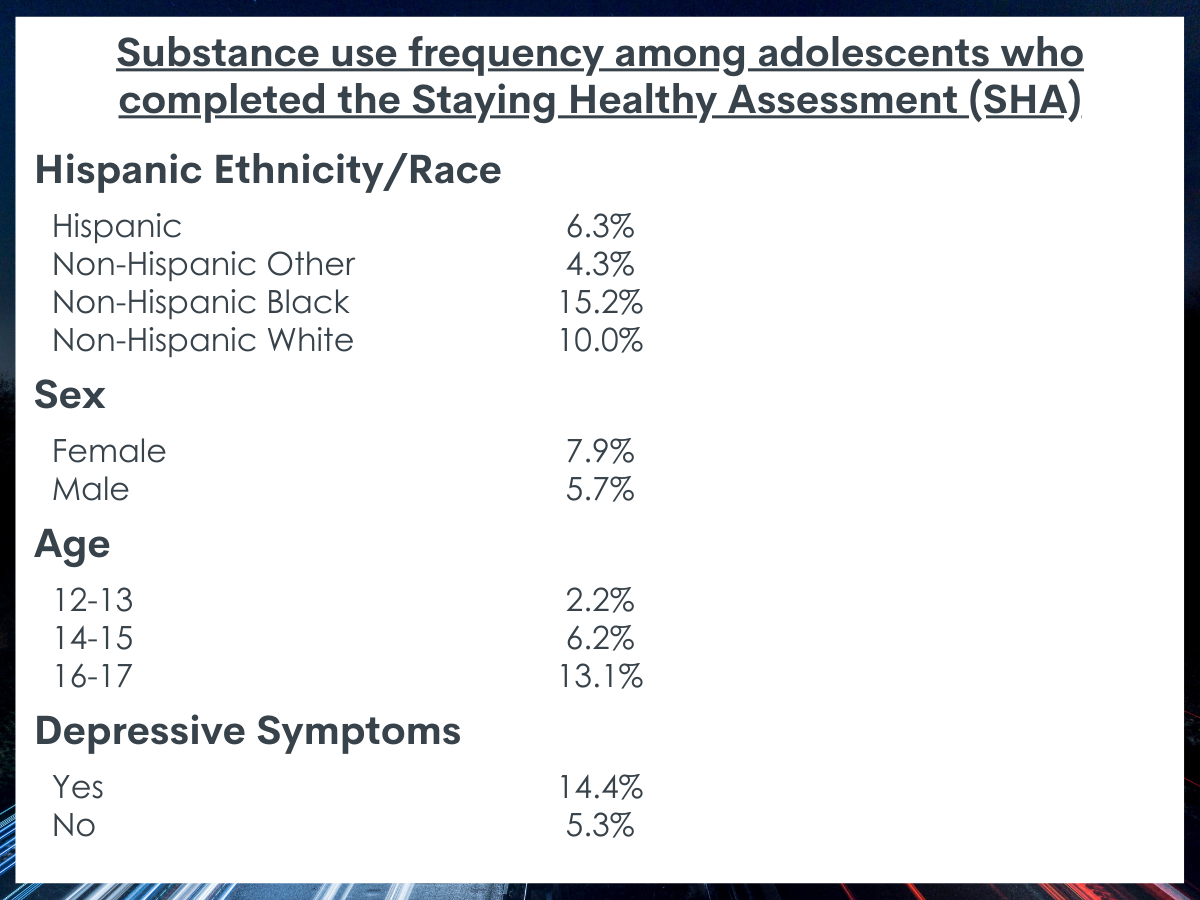
Overall, nearly 7% of youth reported any substance use which varied substantially across age.
Substance use was highest among non-Hispanic black and non-Hispanic white youth compared to the other racial/ethnic categories. Males and females reported similar levels of substance use. Youth with depressive symptoms were more likely than youth without depressive symptoms to report using substances. Adolescents aged 16-17 years old were twice as likely to use substances than a 14-15 year old and nearly 6 times as likely than a 12-13 year old.
Providers felt that youth in their care were not addicted to substances used and that youth who reported use often used substances to address underlying issues.
Providers reported that when they spoke with youth about their substance use, youth often reported using substances to cope with mental health challenges. As a result, providers often viewed screening and follow-up discussions about substance use as a way to identify mental health challenges. Many providers felt that in their experience most youth were not addicted to the substances they used and that most youth who used substances seemed to use cannabis.
The strategies providers reported using when substance use was identified, varied. Some providers reported doing some motivational interviewing with youth, but others also reported referring youth to a behavioral health counselor when they felt the youth was using to cope with mental health challenges or if the use appeared to be heavy and problematic. Ultimately, it seemed that providers’ professional guidelines shaped their views on how important they felt it was to ask youth about their substance use during the clinical encounter.
Providers perceived many structural challenges to consistently using SBIRT in practice.
Providers felt there were a number of challenges that acted as barriers to SBIRT in the clinical setting. First, they discussed a lack of space for confidential substance use and mental health screening with youth apart from their parents, which might lead to dishonest youth answers. They also reported that they might not have the best screening tools. That is, while there are other substance use and mental health screeners for use in the electronic medical record aside from the mandatory Staying Healthy Assessment, these are hard to access or do not fit well into the existing clinical workflow. Finally, they reflected feeling that there was a lack of referral options and they often felt that the system is not set up to support smooth linkages between primary care and substance use treatment options. Many providers were also unclear on how to handle youth with heavy substance use, due to both a lack of standardized guidelines as well as a lack of available addiction treatment options in the area.
Providers suggested taking advantage of technology to support their use of SBIRT and reach more youth.
Providers felt there were several potential solutions to address the different discussed barriers. Overall, they thought that technology-based tools could be better incorporated to support the pre-screening process and linkages to the larger treatment system. Providers felt youth may be more honest with a technology screener on an app. They also felt that if other clinical team members, such as a clinical assistant or nurse could do the screening, it would help save time for the discussion in the clinical encounter. If an automatic flagging system from a substance use screener was in place, this may also save time: the provider could be immediately notified of a substance use issue or, even better, a behavioral health clinician could be notified to come speak to youth at the end of the primary care visit. As well, providers felt that developing an online system where addiction treatment could be easily looked up would help them in providing immediate resources to youth.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Overall, this study of 1436 youth who utilized primary care at a federally qualified health center, reported engaging in less substance use than the national estimates suggest for this age group. Yet, the research team identified discrepancies in use by race/ethnicity, experience of depressive symptoms, and age of youth among this sample. That is, non-Hispanic black youth reported the highest level of substance use. Although black and Hispanic youth may be less likely to be identified and referred to SUD treatment, this study indicates that the prevalence of substance use intervention need might be highest among black youth in this population, suggesting that we may need tailored approaches to reaching these youth. Providers did not seem to address the issue of cultural adaptation for SBIRT in their interview responses, so additional training may be needed in this regard.
Youth who had experienced depressive symptoms also reported higher levels of substance use, compared to youth without such symptoms, a finding similar to previous youth research. And, as would be expected given developmental trajectories, older youth were more likely to report engaging in substance use than younger youth, suggesting screening during primary care visits for this older population of youth is a priority. Indeed, early intervention can be crucial to reducing the risk of developing a substance use disorder and serve to shorten one’s experience with substances and improve one’s health overall.
The 12 providers also identified a number of potential barriers to implementing SBIRT, including from their own skills and knowledge to the available tools and resources provided through the system. One strength of this study is the approach researchers used to ask clinicians about strategies that might help with successfully implementing SBIRT, because clinicians in this setting might be best placed to offer solutions that would work in their setting – that is, whether SBIRT in pediatric primary care is feasible and adoptable. Indeed, these clinicians had several ideas about strategies that could be used to address this gap, including by having more standardized guidelines, using youth-friendly technology such as an iPad to collect data, developing better inter-system linkages through clinical flagging and notification, and further integration of existing tools for screening. For example, there are two youth-validated tools that calculate a risk score and assign SUD risk level could, with clinical support, which be incorporated into the primary care visit: NIDA’s Brief Screener for Tobacco, Alcohol, and Other Drugs and Screening to Brief Intervention. As well, as it ultimately seemed that providers’ professional guidelines shaped their views on how important they felt it was to ask youth about their substance use during the clinical encounter, clinical training should include a focus on risk prevention and how to address questions about youth substance use during a clinical encounter.
These findings suggest that to better identify youth with substance use, more system-level efforts may be needed. That is system-level transformation, or an adolescent-recovery oriented care approach, may be one way to improve the infrastructure for early intervention among young people. The adolescent-recovery oriented care approach conceptualizes the treatment and recovery system as having “no wrong door” to services. Screening, brief intervention, and referral to treatment during a primary care visit is one such door to treatment and recovery services, yet this study indicates that many youth may not have access to this metaphorical door. This is a missed opportunity at the system level that would take coordinated effort to address.
- LIMITATIONS
-
- As these data were collected from youth and providers in an urban setting, the findings may not generalize to challenges in rural settings or in settings with different demographic characteristics.
- Although the measures used to assess substance use and depression symptoms were from measures used throughout the clinical setting, they likely did not necessarily capture the nuance of the youth experience. That is, the depression assessment may be overly sensitive and the substance use questions did not address the level of use (aside from alcohol) or severity of substance used. Vaping behaviors, a rising public health problem in youth, were likely also missed due to the nature of the smoking question. As well, the assessment only captures current behavior, so could be misinterpreted by youth or lead to an underestimate of the extent of youth substance use and depression symptoms.
BOTTOM LINE
In this study of youth who utilized primary care at a federally qualified health center, the researchers found that 7% of the sample overall reported engaging in substance use. Of these youth, there were some large differences in reports of use by race/ethnicity, experience of depressive symptoms, and youth age suggesting that more tailored efforts for screening, brief intervention, and referral to treatment (SBIRT) may be needed to address these large differences within a very narrow age range and period of development. As well, the 12 providers interviewed suggested several system-level barriers to implementing SBIRT, some of which could be addressed with a more supportive infrastructure of training, guidelines, and electronic medical record adaptation.
- For individuals and families seeking recovery: Early screening and intervention can be a crucial first step to preventing adolescent substance use experimentation from developing into a more severe problem. If you are concerned about your child’s substance use, you may be interested in talking to their primary care provider to address this issue in their clinical encounter. There are also available substance use screening tools through the National Institute on Drug Abuse or online government generated resources to identify adolescent-appropriate treatment options.
- For treatment professionals and treatment systems: Early screening and intervention can be a crucial first step to preventing adolescent substance use experimentation from developing into a more severe problem. Conducting formalized screening for substance use and mental health should be an important part of the adolescent clinical encounter as these behaviors and experiences can ultimately influence all other aspects of a young person’s health, including clinical health outcomes. Having an open discussion with youth about their reason for using a substance may also help to identify other problems that could be addressed, for example, if they are using a substance to cope with negative feelings. The National Institute on Drug Abuse has several available screening tools that have been validated with youth, and there is an online government generated resource to identify adolescent-appropriate treatment options to suggest to youth and their families.
- For scientists: Early screening and intervention can be a crucial first step to preventing adolescent substance use experimentation from developing into a more severe problem and the researchers in this study identified a number of future avenues for research to address the barriers to early screening. First, this study could be replicated in different clinical and geographic settings to ensure the findings around youth substance use and SBIRT implementation generalize to these settings or whether there are novel barriers to uncover. As well, focusing on intersectionality, that is, the level of substance use among youth based on several interacting identities (e.g., race/ethnicity, gender identity, sexual identity, etc.) may illuminate further elevated risk and gaps in access to prevention and treatment services. Finally, intervention studies to increase the uptake of SBIRT as a clinical approach in clinical settings seem necessary to close the early intervention-to-treatment gap.
- For policy makers: Early screening and intervention can be a crucial first step to preventing adolescent substance use experimentation from developing into a more severe problem. The researchers in this study found that there is still a high proportion of youth who report using any type of substance and that there may be disparities among youth in receiving the evidence-based screening, brief intervention, and referral to treatment. As well, the researchers found that providers reported several barriers to implementing screening, brief intervention, and referral to treatment, system-level barriers that may be best addressed through a whole system transformational approach through the development of a recovery-oriented system of care. This approach would involve increasing the education and training for providers in implementing screening, brief intervention, and referral to treatment as well as providing structural changes (e.g., to the electronic medical record) to reduce gaps in access to services.
CITATIONS
Yonek, J. C., Velez, S., Satre, D. D., Margolis, K., Whittle, A., Jain, S., & Tolou-Shams, M. (2022). Addressing adolescent substance use in an urban pediatric federally qualified health center. Journal of Substance Abuse Treatment, 135, 108653. doi: 10.1016/j.jsat.2021.108653

