Medications work for criminal justice populations. Is it cost effective?
Medications for opioid use disorder, including buprenorphine/naloxone (i.e., Suboxone) and methadone maintenance, are evidence-based treatments for individuals with opioid use disorder. This study examined also whether such treatments produce ultimate cost benefits.
Little is known about whether Medication Assisted Treatments (MATs) are cost-effective; that is, whether the amount needed to pay for MAT is worth its benefits (e.g., reduced mortality, enhanced abstinence, reduced disease/disability, and reduced crime).
WHAT PROBLEM DOES THIS STUDY ADDRESS?
This study by Gisev and colleagues addressed this question specifically among prisoners in New South Wales, Australia.
HOW WAS THIS STUDY CONDUCTED?
This research study analyzed 16,000 individuals who received Medication Assisted Treatments (MAT) between 1985 and 2010 in New South Wales, Australia, and had at least one prison stay/release between 2000 and 2012.
Among these individuals, 7,857 received Medication Assisted Treatments (MAT) upon release (at release or within 7 days) and 8,116 did not receive MAT; these groups were compared on demographic, criminal justice, and treatment characteristics. In addition, authors used propensity score matching, a statistical technique that helps create two comparable groups, in order to conduct the cost-benefit analysis. Through this strategy, authors ensured that the group of MAT and non-MAT individuals were as comparable as possible in the absence of a randomized design, on predetermined characteristics, including age at release, gender and indigenous status, juvenile justice system history, number of prior offenses, prior MAT engagement, time in jail, and whether released before 2008 (a time when systematic efforts to make MAT more available in the New South Wales prison system were undertaken).
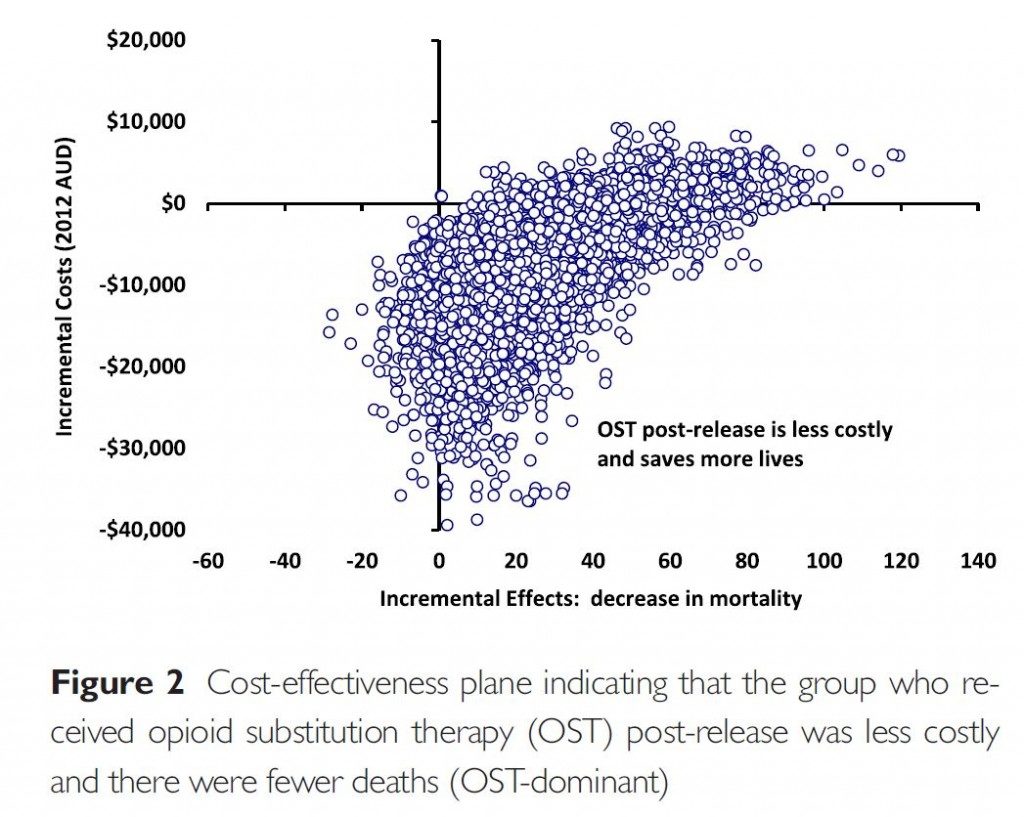
This yielded two matched groups of 6,734 MAT (taking medication for substance use disorder (SUD)) and 6,734 non-MAT (individuals not taking medications for SUD), released from prison to compare costs (treatment, criminal justice, and social costs) and mortality in the 6 months following release from prison. Finally, authors used a “bootstrapping” procedure with 20,000 repetitions, meaning rather than estimate the effects purely from the two matched samples, they take smaller random samples of the overall sample (6,734 and 6,734) and carry out the analyses 20,000 times. This way they were able to determine how variable and reliable the results were. This is considered to be a rigorous statistical approach, and is contrasted with a conventional inferential approach, where the conclusion is that the group difference observed “is very unlikely due to chance”.
WHAT DID THIS STUDY FIND?
The Medication Assisted Treatments (MAT) group had a greater proportion of individuals that were: female & indigenous, more likely to have prior offenses, a juvenile justice history, & receive medications in prison.
Using the matched groups, the Medication Assisted Treatments (MAT):
- Cutback the liklihood of death by 50% (20, or 0.3% for MAT vs. 46, or 0.7% for non-MAT) &
- Only cost society half as much during this time (roughly $7000 MAT vs. $14,000 for non-MAT per individual)
The cost-effectiveness ratio (difference between groups in costs divided by difference between groups in deaths; i.e., cost per year of life gained) was -1400$, suggesting Medication Assisted Treatment (MAT) was the dominant strategy.
Building on prior studies which have shown Medication Assisted Treatment (MAT) is effective in enhancing abstinence and other positive health outcomes, this health economics study indicates that MAT is also a cost-effective approach for recently released prisoners with opioid use disorders.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Opioid use disorders cost U.S. taxpayers billions of dollars annually.
It is important to examine the cost related to the salutary impact of addiction treatment. Such analyses can enhance the rationale for increased funding and health care coverage dedicated to the treatment and ongoing recovery management of substance use disorders.
Although research using other relevant populations and settings are needed, the implications of this study are potentially large and far-reaching:
- Medications are effective for substance use disorder (SUD) remission
- Medications are cost-effective with respect to impact on reduced mortality in criminal justice populations
Among those released on medication, approximately 95% were on Medication Assisted Treatment (MAT) while in prison. This suggests interventions that help prisoners access medications substantially increases the likelihood they will engage with medications upon release or shortly after leaving prison.
- LIMITATIONS
-
- The interpretations and implications of the study are constrained by the specifics of the sample and setting – prisoners in New South Wales, Australia, that have been on Medication Assisted Treatment (MAT) before. Although individuals could not be randomized to MAT vs. no MAT, sophisticated statistical approaches, including propensity score matching with bootstrapping, helped reduce the likelihood that some other variable is accounting for the observed effects (e.g., more extensive criminal justice histories), and helped isolate the effect of MAT.
NEXT STEPS
Next steps are to examine the cost effectiveness of Medication Assisted Treatment (MAT) not only with respect to life years gained, but also quality life years gained as is typically done.
BOTTOM LINE
- For individuals and families seeking recovery: For opioid users released from prison, medications may have a positive impact and could potentially save lives.
- For scientists: This methodologically sound study may serve as a model for future similar studies of the cost effectiveness of pharmacological and psychosocial addiction interventions, especially where the independent variable is not directly under the researcher’s control.
- For policy makers: Consider funding to help prisoners access Medication Assisted Treatment (MAT) during their sentence and/or upon their release. This study shows every $500 invested in medication treatments is likely to save 1 year of life.
- For treatment professionals and treatment systems: Interventions that help prisoners access Medication Assisted Treatment (MAT) during their sentence enhances the likelihood that they will access MAT upon their release, a cost-effective way to increase their chances of survival. OST is also an effective treatment for opioid addiction in its own right, and may serve as an important intervention that can help opioid addicted prisoners stabilize and successfully re-enter society upon release.
CITATIONS
Gisev, N., Shanahan, M., Weatherburn, D. J., Mattick, R. P., Larney, S., Burns, L., & Degenhardt, L. (2015). A cost-effectiveness analysis of opioid substitution therapy upon release in reducing mortality among prisoners with a history of opioid dependence. Addiction. doi:10.1111/add.13073
Image Source: http://www.tampabay.com/news/courts/criminal/aging-popluation-takes-toll-on-us-prisons/2228081

