Predicting Treatment Dropout with Cortisol Levels & Reported Stress
Methadone maintenance treatment (MMT) is an evidence-based medication treatment for individuals with opioid use disorders. Increased emotional distress, often but not always in the context of a co-occurring psychiatric disorder, however, can make treatment more challenging.
The impact of stress on methadone maintenance engagement is not well understood to this point.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Jaremko and colleagues used both self-report and physiological measures of stress to examine its potential influence on Methadone Maintenance Treatment (MMT) engagement.
HOW WAS THIS STUDY CONDUCTED?
Authors sought to examine:
a) whether Methadone maintenance treatment (MMT) patients had different stress levels than non-opioid dependent controls, recruited from faculty and students at the university where the study was conducted
b) differences in stress and other clinical variables (e.g., withdrawal symptoms) between Methadone maintenance treatment (MMT) drop-outs and those that were maintained during the first 6 months of treatment
c) the best predictors of treatment engagement/discontinuation
Stress was measured by self-report (with the perceived stress scale and civilian PTSD check list) and objectively by saliva cortisol level at treatment intake. Regarding cortisol level, authors classified individuals into two groups, normal cortisol or abnormal cortisol level. An “abnormal” level in Methadone maintenance treatment (MMT) patients was defined as one standard deviation above or below the mean for controls (2.39-6.39 nmol/L was the normal range).
WHAT DID THIS STUDY FIND?
Results showed that Methadone maintenance treatment (MMT) participants had significantly more perceived stress and PTSD symptoms.
NOTABLY FROM THE STUDY, Methadone Maintenance Treatment (MMT) Participants:
- had greater cortisol levels; consistent with how abnormal cortisol was defined (one standard deviation above or below the average control participant level)
- almost 60% had a PTSD symptom score of 45 or greater, which is the scale cut-off for a PTSD diagnosis, suggesting many MMT patients likely met diagnostic criteria for clinically significant PTSD
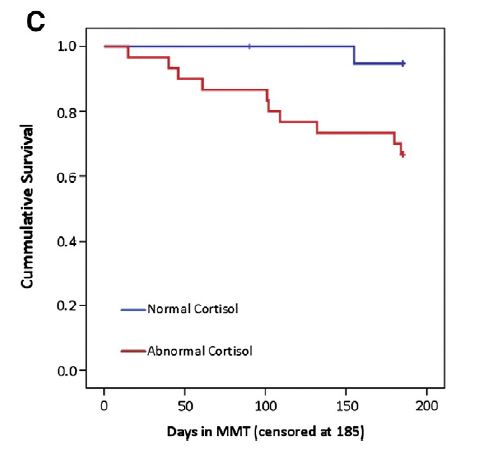
Regarding differences between individuals still in MMT at 6 months and those who were no longer in treatment (drop-out, death, jail, asked to leave program), non-completers had similar self-report measures of stress, but greater likelihood of abnormal cortisol (91% vs. 51%).They also evidenced greater withdrawal symptoms, more opioid use, poorer medication compliance, and less group therapy attendance.
In analyses predicting days in methadone maintenance treatment (MMT), treatment discontinuation, and time to discontinuation by 6 months, also controlling for confounding variables (demographics and substance use variables), abnormal cortisol level was the best, and often only, significant predictor.
Of note, in predicting days in Methadone maintenance treatment (MMT), the effect of perceived stress only in those with abnormal cortisol levels, just missed statistical significance, suggesting both self-report and objective bio-markers of stress may be important to assess.
Study findings suggest that a thorough assessment of Methadone maintenance treatment (MMT) patients’ stress levels when they are initially admitted to treatment may help identify individuals at particularly high risk of dropping out of treatment prematurely.
WHY IS THIS STUDY IMPORTANT
Research that examines the impact of stress from multiple perspectives can help programs identify strategies to screen individuals at risk of drop-out and inform interventions that address this magnified drop-out risk.
Although follow-up studies are needed, this study suggests:
a) stress is important to measure in Methadone maintenance treatment (MMT) patients upon admission, and may help predict drop-out risk
b) stress should be measured with subjective (e.g., perceived stress) and objective measures (e.g., cortisol)
c) given the high PTSD symptom scores in MMT patients, treatment providers may wish to screen specifically for the presence of PTSD & refer patients to trauma informed care
- LIMITATIONS
-
- The sample was small (58 patients) and from a single treatment program. As mentioned by the authors, those that agreed to take part in the study were less likely to have a history of poly-drug use and had fewer legal problems relative to those who declined to participate. It is unclear whether these results generalize to other programs and populations of Methadone maintenance treatment (MMT) patients.
- In addition, authors conducted dozens of statistical analyses without controlling for multiple tests inflating the overall type I error rate (i.e., increasing the probability of finding a significant result due to chance). Although results should be taken with caution and possibly considered exploratory at this stage, findings generally supported the role of cortisol levels in explaining Methadone maintenance treatment (MMT) patient engagement across analyses. This increases confidence that this physiological stress marker may be clinically relevant in MMT.
NEXT STEPS
Follow-up on this unique clinical study would ideally involve a larger sample of Methadone maintenance treatment (MMT) patients across several programs to determine whether these findings are replicable.
If replicable, subsequent studies may examine the feasibility of measuring saliva cortisol levels in clinical programs and may test interventions to address these elevated stress levels that might mitigate drop-out (e.g., mindfulness strategies).
BOTTOM LINE
- For individuals & families seeking recovery: Experiencing stress in the body can affect the likelihood of remaining in treatment even if one is not completely aware of it.
- For scientists: More research is needed to examine the generalizability of the current study before definitive conclusions can be offered.
- For policy makers: Consider increased funding for research on multi-modal measurement of addiction-related phenomena, such as physiological markers of emotional stress. They might help clinical scientists better understand treatment response and identify people at risk of drop-out ahead of time.
- For treatment professionals and treatment systems: You may consider a more thorough bio-psycho-social evaluation of your patients’ stress levels at intake and use those clinical data to inform treatment planning (e.g., adjunctive therapy for PTSD).
CITATIONS
Jaremko, K. M., Sterling, R. C., & Van Bockstaele, E. J. (2015). Psychological and physiological stress negatively impacts early engagement and retention of opioid-dependent individuals on methadone maintenance. J Subst Abuse Treat, 48(1), 117-127. doi:10.1016/j.jsat.2014.08.006

