Promising 12-step Facilitation Treatment for Patients With Co-occurring Disorders
Research has shown treatments that help increase participation in groups like Alcoholics Anonymous & Narcotics Anonymous result in greater likelihood of abstinence and remission for those with substance use disorder.
For patients who have another co-occurring psychiatric disorder, especially if the other psychiatric disorder is debilitating, such as psychotic disorder or chronic major depressive disorder, studies have also shown that participation in 12-step mutual-help organizations that focus on both severe mental illness & addiction are associated with better outcomes.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Consequently, in this study, Bogenschutz and colleagues tested the added clinical benefit of proactively facilitating participation in Double Trouble in Recovery (DTR) by adapting a Twelve-Step Facilitation (TSF) treatment for patients with a co-occurring alcohol use disorder (AUD) and severe mental illness, including bipolar disorder, major depressive disorder, or psychotic disorder, who were attending outpatient treatment.
HOW WAS THIS STUDY CONDUCTED?
The research team randomized 121 individuals with alcohol use disorder (AUD) and co-occurring psychotic (18%), bipolar (36%), or major depressive disorder (46%) attending an outpatient program that caters specifically to individuals with co-occurring disorder to receive treatment as usual (TAU; n = 38) by itself, or with an add-on Twelve-Step Facilitation (TSF) intervention designed specifically for patients with severe co-occurring disorders (n = 83).
The Twelve-Step Facilitation (TSF) treatment, adapted from the TSF intervention used in another large treatment study called Project MATCH, was tailored for those with co-occurring disorders by emphasizing:
- Double Trouble in Recovery (DTR) rather than Alcoholics Anonymous (AA) for recovery support
- The impact of psychiatric illness on one’s addiction
- Remaining engaged with psychiatric treatment
- Social skills training to prepare patients for the 12-step social milieu
- Transportation assistance to and from Double Trouble in Recovery (DTR) meetings and therapy appointments
- Active linkage with a current member of Double Trouble in Recovery (DTR) with 1+ years of continuous abstinence who attended the second session of treatment
The patients not randomized to receive the adapted Twelve-Step Facilitation (TSF) received only treatment as usual (TAU), which consisted of medication monitoring, individual therapy, and case management. In other words, all patients received treatment as usual (TAU), but TSF patients also received the intervention to encourage Double Trouble in Recovery (DTR) attendance. Even though groups were randomized in such a way as to attempt to equate them on a number of characteristics so that the only thing that differed between the groups was whether they got TSF or not, the group of patients assigned to the TSF intervention, on average, still had greater alcohol abstinence and a higher percentage of individuals with another drug use disorder (e.g., marijuana) in addition to alcohol use disorder (AUD) at the start of treatment, which the authors mention in their study limitations.
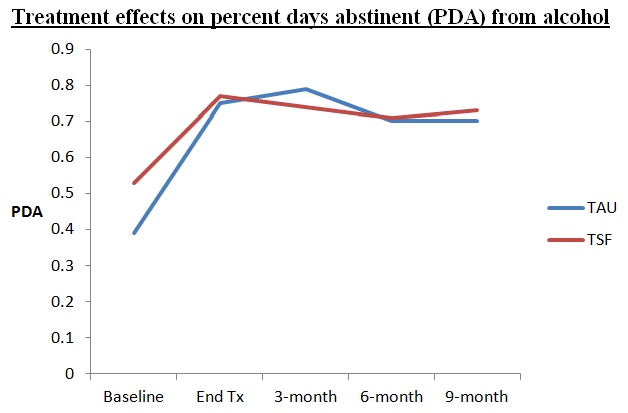
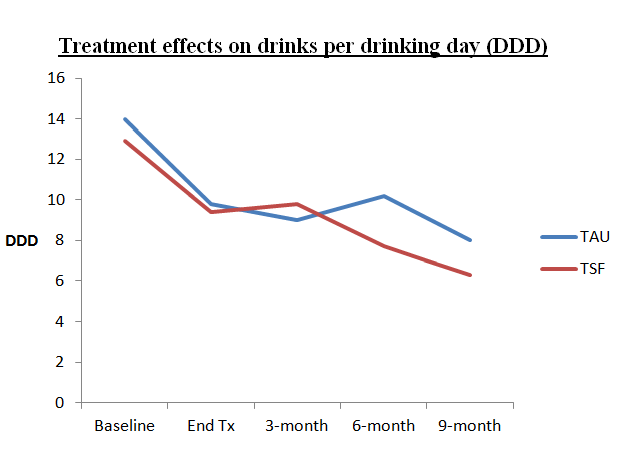
The main clinical outcomes (measured at the end of treatment (12 weeks), and 3-, 6-, and 9-month follow-up assessments) examined were:
- percent days abstinent from alcohol (PDA)
- drinking intensity (i.e., drinks per drinking day, or DDD)
Researchers tested whether Twelve-Step Facilitation (TSF) participants had significantly greater increases in percent days abstinent from alcohol (PDA) and significantly greater decreases in drinking intensity (DDD) during treatment and at the 9-month follow-up compared to patients receiving only TAU.
Researchers used the 12-step Participation Questionnaire to measure participants’ completion of 12-step work in addition to other central 12-step activities and beliefs including having a sponsor and considering oneself a 12-step member. Finally, it is worth highlighting the staff therapists were very well trained in the delivery of Twelve-Step Facilitation (TSF) before the study, including an intensive training period with feedback provided on videotaped sessions by the developer of Project MATCH’s TSF. Feedback was also provided to therapists during the study, and trained coders found that therapists, on average, demonstrating about 90% of the identified “ingredients” of TSF each session, suggesting they delivered the treatment as designed.
WHAT DID THIS STUDY FIND?
Compared to treatment as usual (TAU) patients, Twelve-Step Facilitation (TSF) patients:
- were more likely to attend a 12-step meeting during treatment (66% vs. 30%) including Double Trouble in Recovery (DTR) and traditional 12-step meetings, such as AA
- attended a higher number of 12-step meetings during treatment (11 vs. 3 percent days attending a meeting)
- reported greater levels of 12-step activities/beliefs both during treatment and at 9-month follow-up
Despite their greater participation in 12-step groups, Twelve-Step Facilitation (TSF) patients and treatment as usual (TAU) patients had similar positive changes in percent days abstinent from alcohol (PDA) and DDD during treatment, that were maintained, on average, by the 9-month follow-up with no group differences. They also had similar percentage of days taking their prescribed psychiatric medication and attendance at psychiatric treatment sessions. Because Twelve-Step Facilitation (TSF) promoted more 12-step attendance, but participants only attended 5 of 12 sessions on average, the researchers examined whether greater participation in TSF was associated with better outcomes.
More Twelve-Step Facilitation (TSF) treatment sessions attended were associated with better percent days abstinent from alcohol (PDA) & drinking intensity (DDD) during treatment and at the 9-month follow-up.
Several important contributions of this study:
- First, in this sample of patients with co-occurring alcohol use disorder (AUD) and psychiatric disorders including psychotic, bipolar, and major depressive disorder, 12-step mutual-help attendance across all types of organizations (including both AA & Double Trouble in Recovery (DTR)) was associated with better percent days abstinent from alcohol (PDA) and drinking intensity (DDD), irrespective of treatment group, raising confidence in clinical referral to 12-step groups for this patient group. This supports other research studies that have found that patients with a range of co-occurring disorders can do well in groups such as AA and NA (see here, for example).
- Second, an intervention designed specifically for individuals with co-occurring disorders, including an emphasis on Double Trouble in Recovery (DTR) – the most well known 12-step group for these individuals – may promote increased 12-step participation, which appears to be maintained well after treatment delivery (up to 9 months afterward).
- Third, consistent with previous studies, adults with co-occurring disorders present unique challenges. These patients attended, on average, only 5 of 12 Twelve-Step Facilitation (TSF) sessions (compared to 8 of 12, on average, among substance use disorder (SUD)-only patients in Project MATCH), and maxed out at 11% days attending a community 12-step meeting (compared to more than 20% during treatment among SUD-only patients in Project MATCH). An intensive, tailored intervention for this group including peer linkage and transportation to meetings appeared to be an effective strategy, though more innovative approaches may be needed to increase their treatment participation.
As noted above, each additional Narcotics Anonymous (NA) meeting attended per week was associated significantly with a 2% increase in the odds of treatment retention and a 1% increase in the odds of abstinence at 6 months. Negative attitudes toward buprenorphine may begin to shift as medication-assisted treatment becomes more widely accepted as an evidence-based treatment for people seeking recovery.
Also, in a time-lagged analysis that investigated the combined influence of 12-step attendance for the whole sample (i.e., regardless of which treatment they received) across the entire 1-year study period, where 12-step attendance at one time point predicted alcohol outcome at the next time point (e.g., baseline attendance on end-treatment outcomes, end-treatment attendance on 3-month follow-up, 3-month follow-up on 6-month outcomes, etc.), 12-step attendance was associated both with better percent days abstinent from alcohol (PDA) and drinking intensity (DDD).
WHY IS THIS STUDY IMPORTANT
Twelve-Step Facilitation (TSF) for patients with co-occurring alcohol & severe psychiatric disorder could be a valuable clinical intervention to improve quality of life & ability to function in the community.
This Twelve-Step Facilitation (TSF) intervention tailored specifically for patients with co-occurring alcohol and severe psychiatric disorder, with many innovative adaptations (e.g., in-session peer linkage), may promote increased 12-step participation. To date, it is the only known TSF intervention designed specifically for this patient group with severe mental health problems.
- LIMITATIONS
-
- The primary limitation is that analyses combined all 12-step participation, so we cannot say what proportion of patients’ attendance was to Double Trouble in Recovery (DTR), and what proportion was to traditional 12-step mutual-help groups, like AA or NA.
- Another issue is specific to the post-hoc analyses examining whether more Twelve-Step Facilitation (TSF) participation is associated with better outcomes. While one interpretation may be that patients need to receive a sufficient “dose” of TSF to derive maximum benefit, these analyses did not control for other individual traits associated with better outcomes (e.g., abstinence motivation), like the main TSF vs. treatment as usual (TAU) analyses which equalized groups on these characteristics through the randomization procedure described in “What did this study do?” Therefore, the positive impact of more TSF sessions attended could be explained by the influence of another factor like greater motivation and/or having more recovery resources, rather than the benefits of attendance per se. Further research should try to tease these effects apart.
NEXT STEPS
An interesting next step would be to test if group versus individual Twelve-Step Facilitation (TSF) for those with co-occurring disorders, or to add a second treatment group to test whether incentivizing treatment attendance could lead to better outcomes:
Twelve-Step Facilitation (TSF) + Contingency Management VS. Twelve-Step Facilitation (TSF) VS. treatment as usual (TAU)).
BOTTOM LINE
- For individuals & families seeking recovery: If one has co-occurring alcohol use and psychiatric disorders, participating in an add-on Twelve-Step Facilitation (TSF) intervention tailored for his/her clinical needs, which emphasizes meetings that cater to those with co-occurring disorders could help them become more involved in these community organizations and thereby have better outcomes.
- For scientists: This randomized trial for patients with co-occurring disorders in outpatient treatment found similar outcomes for those who received an adapted 12-step facilitation and those who did not. One of the challenges is that patients in TAU often also attend 12-step meetings even when that may not be emphasized as part of their intervention. This means that patients in both conditions make use of these free community recovery resources which can wash out any treatment differences. Limitations in the current study include a clinical focus on Double Trouble in Recovery (DTR) but measurement of 12-step participation more generally, and an inability to determine whether more treatment engagement actually predicts better outcomes because these analyses did not control for factors that could predict both treatment engagement and better outcomes (e.g., abstinence motivation), and might be responsible for the effect researchers observed. These limitations should be examined in future research.
- For policy makers: Despite null findings, there were many encouraging results in this trial of Twelve-Step Facilitation (TSF) for patients with co-occurring psychiatric disorders, including the fact that community participation in 12-step meetings was associated with better outcomes. Consider continued funding for this line of research.
- For treatment professionals and treatment systems: For your patients with co-occurring alcohol use and psychiatric disorders, providing an add-on 12-step facilitation tailored specifically for them that emphasizes meetings which cater to those with co-occurring disorders could facilitate their involvement in these community organizations and produce better outcomes.
CITATIONS
Bogenschutz, M. P., Rice, S. L., Tonigan, J. S., Vogel, H. S., Nowinski, J., Hume, D., & Arenella, P. B. (2014). 12-step facilitation for the dually diagnosed: a randomized clinical trial. J Subst Abuse Treat, 46(4), 403-411. doi: 10.1016/j.jsat.2013.12.009

