Promising evidence that mobile engagement units can link hard-to-reach individuals with opioid use disorder to medication treatment
Opioid-related overdose deaths are an going public health crisis in the United States, and a large majority of individuals with opioid use disorder do not receive first-line treatment with medications. Interventions that overcome barriers and link people to evidence-based treatments are a critical component of addressing the opioid crisis. In this study, a mobile engagement unit was evaluated to see if this intervention would improve treatment utilization among a hard-to-reach population.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Drug overdose deaths have risen to historically high levels, approaching 100,000 lives lost in a 12-month period ending in March 2021. A large majority of these overdose deaths are opioid-related. Medications are first-line treatment for opioid use disorder and have been shown to decrease mortality. Despite this evidence, it is estimated that 20% of individuals with opioid use disorder receive medication treatment, highlighting a large treatment gap. Patient barriers to engaging in treatment include stigma, transportation, limited readiness to change, negatives attitudes or beliefs about treatment, and treatment costs. Novel interventions have emerged to address these barriers and to link individuals with opioid use disorder to evidence-based treatment, such as post-overdose response teams, peer outreach, and mobile units.
Recently, mobile units, an alternative model of healthcare delivery typically using a van or a bus, have been implemented in urban areas in the United States as an innovative way to bring treatment services to hard-to-reach populations, such as injection drug users, people experiencing homelessness, and the uninsured. Mobile units are uniquely equipped to go directly into areas where these vulnerable populations congregate and often offer a variety of services. However, empirical research for the effectiveness of these interventions is limited. In this study, researchers examined the effectiveness of a mobile engagement unit in Philadelphia to connect individuals with opioid use disorder to a methadone treatment program. Results from this study provide crucial empirical data to evaluate this type of novel intervention and help inform the potential widespread implementation of these programs to address the drug overdose public health crisis.
HOW WAS THIS STUDY CONDUCTED?
This study compared the effect of a mobile engagement intervention with traditional intake pathways on treatment utilization among Medicaid beneficiaries at a methadone treatment center in Philadelphia. Study participants were enrolled from October 2018 to March 2019 and Medicaid claims data and treatment data were used to assess treatment utilization before and after an initial intake appointment.
The mobile engagement unit that served as the intervention in this study provided a one-time transportation for study participants to a methadone clinic for an evaluation and often same-day initiation of methadone treatment.
In other words, the mobile unit did not initiate medications and did not provide regular transportation to and from the methadone clinic but served as a one-time linkage to treatment.
The mobile unit was staffed by two certified peer specialists and a licensed social worker and operated in neighborhoods with high opioid overdose rates in Philadelphia. There was also a third peer specialist that coordinated with law enforcement to identify areas where the mobile unit should be dispatched. Other services provided by the mobile unit included providing help and information to meet basic needs of clients, distributing naloxone, developing rapport with clients, and identifying and meeting individuals in need via a toll-free telephone number.
The design of the study was a retrospective cohort study, meaning that researchers looked back at the data to see how exposure to a mobile engagement unit affected treatment utilization outcomes. Clients who were referred to the methadone clinic through more traditional pathways, such as walk-ins, treatment referrals, and court orders, served as a comparison group. The researchers used Medicaid claims data to capture sociodemographic factors, clinical characteristics, and treatment utilization measures, and treatment data at the methadone clinic to identify the referral source (mobile unit vs. traditional referral pathway). Sociodemographic factors included age, race, gender, and Supplemental Security Income (SSI) disability status, while clinical characteristics included presence of a psychiatric diagnosis, substance use diagnosis, or both.
In terms of main study outcomes evaluated, the study assessed three substance use treatment utilization measures over three months after individuals attend an initial intake appointment at the methadone clinic: methadone maintenance services, intensive outpatient services, and outpatient services. These treatment outcomes were dichotomized as Yes/No, meaning that an individual using one of these services at least once in the three-month period was coded as “Yes.”
To compare the treatment utilization outcomes for the mobile engagement versus comparison condition, the research team examined the change in treatment engagement – for each of the three outcomes – from the 3 months before their intake appointment to the 3 months after their intake appointment. They then tested whether the mobile engagement group showed a different degree of change (i.e., greater increase) over time than the comparison group. For these primary analyses, they adjusted statistically for demographic and clinical factors that predicted the treatment utilization outcomes to isolate, as best they could, the effect of attending the intake appointment through the mobile unit or other means.
A total of 468 Medicaid beneficiaries enrolled in treatment at the methadone clinic from October 2018 to March 2019, with 53 of these individuals being transported by the mobile engagement unit and 415 individuals coming to the clinic through more traditional pathways.
The treatment and comparison groups had similar demographic and clinical characteristics, with the latter specifically represented by these two groups having similar rates of the presence of codes in Medicaid claims data for substance use and psychiatric diagnoses. The only measured difference was that the treatment group had a higher proportion of individuals identified as white (64% vs. 43%) and a lower proportion of individuals identified as Black (17% vs. 44%).
WHAT DID THIS STUDY FIND?
Treatment utilization measures before intake were higher among traditional referrals.
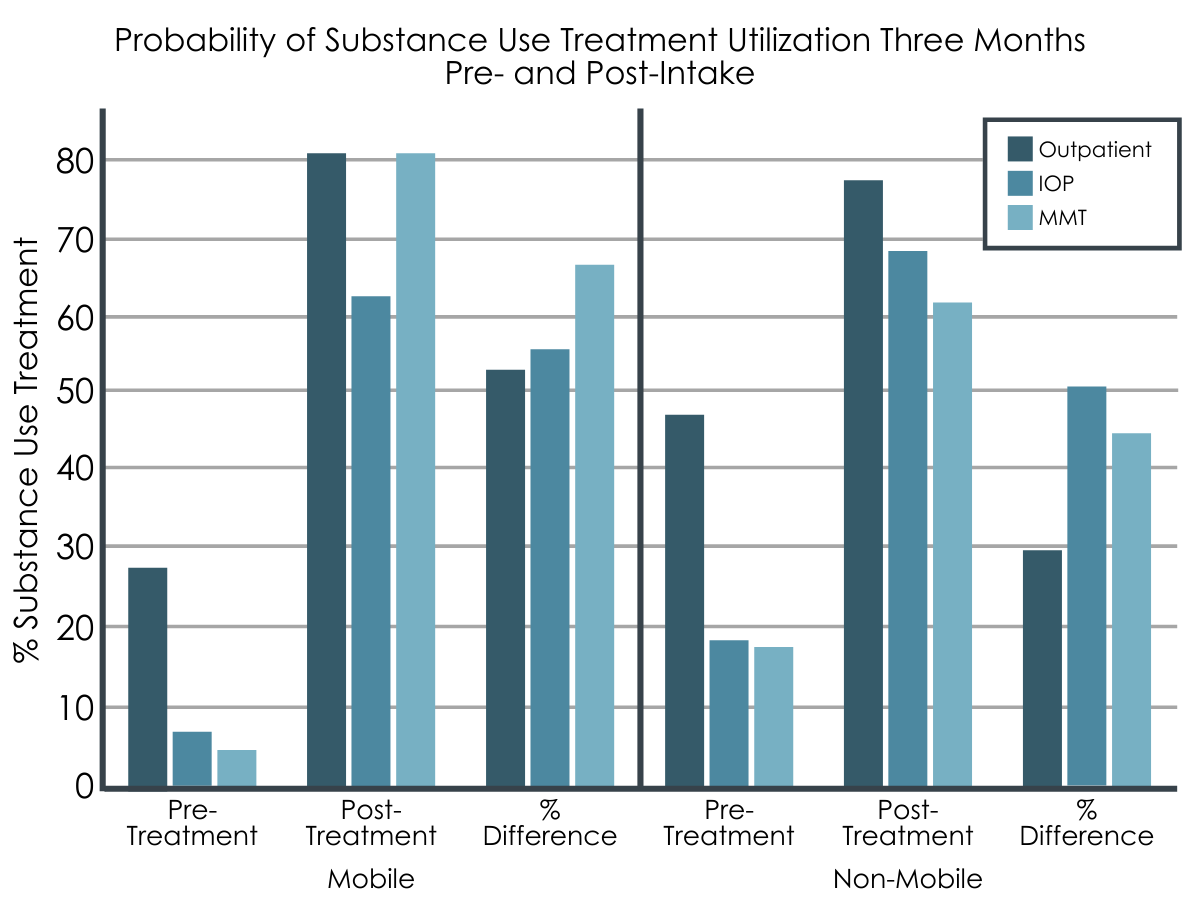
In the three-month period before treatment intake at the methadone clinic, 27.8%, 7.7%, and 4.5% of mobile engagement unit referral group and 47.3%, 18.7%, and 18.0% of the traditional referral group had used outpatient, intensive outpatient, and methadone maintenance services, respectively.
Treatment utilization measures after intake were similar among the two groups.
In the three-month period after treatment intake at the methadone clinic, 80.6%, 63.3%, and 80.3% of the mobile engagement unit referral group and 77.0%, 68.9%, and 62.2% of the traditional referral group had used outpatient, intensive outpatient (IOP), and methadone maintenance services (MMT), respectively.
There was an increase in treatment utilization measures attributable to the intervention.
The mobile engagement unit intervention was associated with a 23-percentage point increase in the probability of using outpatient services and a 32-percentage point increase in the probability of methadone maintenance services compared with the traditional referral group. The relative increase among the mobile engagement unit referrals for utilizing intensive outpatient services (5 percentage points) was not statistically significant.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study linked Medicaid claims data and treatment data to examine the effect of a mobile engagement unit intervention on subsequent treatment utilization. Individuals who were referred by the mobile unit were more likely to use methadone maintenance and outpatient services after intake compared to individuals who were referred through more traditional pathways.
As overdoses continue to rise in the United States and the majority of individuals with opioid use disorder not receiving evidence-based treatment with medications, innovative interventions that can link people to this type of treatment have become a crucial component in solving the opioid overdose crisis. Findings from the study showed that a more assertive outreach approach via a mobile engagement unit intervention, where individuals were provided with one-time transportation to a methadone clinic, not only linked a hard-to-reach population to a methadone program intake appointment but also increased the likelihood of subsequent treatment utilization over a three-month period relative to entering treatment through more traditional pathways, such as walk-ins, referrals from treatment providers, and court orders. The observed benefit of this one-time linkage to the methadone program was a surprising finding to researchers because prior evidence for mobile units that provided repeated transportation to treatment has been mixed.
This mobile engagement unit intervention is uniquely positioned to capitalize on the window of opportunity for engaging in treatment, which may explain the increase in subsequent treatment utilization. Not only does the mobile intervention make treatment accessible in the communities that it serves, but the telephone component of the intervention allows individuals to be quickly reached that are seeking treatment. Having a social worker coordinating with law enforcement to identify opioid overdose hotspots may further enhance the intervention. This type of intervention that links individuals with opioid use disorder to treatment may have advantages over other interventions, such as post-overdose response teams and emergency department-initiated buprenorphine, where a prerequisite to the intervention is generally an opioid overdose or other opioid-related harm. Thus, this mobile outreach shows the potential to engage people without waiting for an adverse overdose event to occur.
Another component of the mobile engagement unit intervention that may have improved outcomes is the utilization of certified peer specialists with lived experience. Since the intervention involved harm reduction services and meeting the basic needs of individuals in the communities it serves on a repeated basis, the mobile unit staffed by peers had an opportunity to engage in relationship-building through a nonjudgmental and unconditional approach, which could have encouraged these individuals to eventually seek and engage in treatment. Peers with lived experience have been shown to improve treatment outcomes in a variety of settings.
Another reason that there may have been differences in treatment utilization between those referred by the mobile engagement unit and those referred by more traditional pathways is that the former were predominantly white individuals (64%) and the latter had a large Black population (44%). Previous research has shown that white individuals were more likely to receive buprenorphine prescriptions than Black individuals, and that Black individuals were less likely than white individuals to complete addiction treatment. Although a statistical technique was used to adjust for racial differences, it is possible that unmeasured differences associated with race/ethnicity, such as differences in recovery capital, may have accounted for the greater service use increase in the mobile engagement unit group.
Findings from this study provided empirical data on accessing subsequent treatment after being evaluated for methadone treatment but did not measure treatment engagement or treatment retention, which would be assessed through the frequency of treatment utilization. Future studies should assess treatment engagement and retention in addition to treatment access. In addition, future studies may explore patient experiences and patient-reported outcomes through qualitative research, which may provide more insight to these surprising study findings. Research into mobile interventions is especially relevant given a new rule from the Drug Enforcement Agency that will allow Opioid Treatment Programs to establish and operate mobile methadone vans, where methadone can be administered on site, without obtaining a separate DEA registration for each mobile component.
- LIMITATIONS
-
- Study participants were not randomized to receive the mobile engagement unit intervention. Therefore, it is possible that other factors beyond the mobile intervention itself could be explaining the improvements in treatment engagement in the mobile intervention group.
- This study was done in a large urban city in the United States and only connected individuals to one type of medication for opioid use disorder treatment. In addition, the mobile engagement unit provided one-time transportation to treatment and did not deliver medication treatment via the mobile unit. Generalizing these results to other areas and other mobile interventions should be done with caution.
- This study used a dichotomized outcome variable for treatment utilization and did not provide information on how often services were being utilized. Therefore, the outcome was a proxy for access to treatment and not retention in treatment. In addition, individuals were only retrospectively followed for a three-month period. Longer prospective studies that measure access, engagement, and retention in treatment are important in further studying this intervention.
- An assumption that must be met in a difference-in-difference analysis is parallel trends, which means that treatment and control groups were on the same trajectory prior to the intervention. Authors state that this assumption was met but do not provide details or a visual depiction of this assumption, which is usually standard in this type of study.
- The mobile intervention treatment group had more room for improvement compared with the comparison group given that they started with lower treatment utilization measures in the pre-period.
- This study did not stratify results based on the type of referral for individuals entering methadone treatment through the traditional pathway. If most of these individuals were entering treatment because of a court order, there may be significant differences in motivation between the treatment group and the comparison group that are unaccounted for in the analysis.
BOTTOM LINE
This study linked Medicaid claims data and treatment data to examine and begin to estimate the effect of a mobile engagement unit intervention, where individuals were provided with one-time transportation to a methadone clinic in Philadelphia, on subsequent treatment utilization. Individuals who were transported to treatment services via the mobile unit were more likely to use methadone maintenance and outpatient services after intake compared to individuals who were referred through more traditional pathways. This assertive outreach intervention is noteworthy in that it does not wait for an adverse overdose or other event to occur before intervening; thus, it has the potential to save more lives and exert greater public health impact.
- For individuals and families seeking recovery: Findings from this study suggest that a mobile engagement unit targeting at-risk areas and individuals may be a promising strategy to initiate methadone treatment among individuals with an opioid use disorder and may improve subsequent treatment utilization. Individuals with opioid use disorder are at very high risk for overdose and other opioid-related harm, especially in the context of an illicit opioid supply where fentanyl is pervasive. Medication treatment has been shown to reduce mortality and improve other treatment outcomes. Despite this evidence, most individuals with this disorder are not treated with these medications.
- For treatment professionals and treatment systems: Findings from this study suggest that a mobile engagement unit targeting at-risk areas and individuals may be a promising strategy to initiate methadone treatment among individuals with an opioid use disorder and may improve subsequent treatment utilization. Linking people to medication treatment is a crucial component to solving the opioid crisis, as most individuals with opioid use disorder are not treated with these medications despite strong evidence that receiving these medications is associated with reduced mortality and opioid use. Although there may be several reasons for why this intervention increased subsequent treatment utilization, more assertive outreach via mobile units is emerging as an innovative way to link people to treatment or deliver services. Many interventions that link people to treatment involve intervening shortly after an overdose, making mobile units especially desirable given that this is not a prerequisite to the intervention.
- For scientists: Findings from this study provided empirical data on accessing subsequent treatment after being evaluated for methadone treatment but did not include continuous measures of treatment engagement or treatment retention. Overall, more rigorous evaluation of this and other mobile outreach interventions are needed given the imperfect study design and the potential for unmeasured confounding. Future studies should assess treatment engagement and retention in more detailed and nuanced ways. In addition, future studies may explore patient experiences and patient-reported outcomes through qualitative research, which may provide more insight to these somewhat unexpected study findings. This study was done in the urban area of one city and predominantly served white individuals, so future studies that include different geographical and demographic groups would be beneficial to this emerging field. In addition, individuals were only retrospectively followed for a three-month period. Longer prospective studies that measure access, engagement, and retention in treatment are important in further studying this intervention. Research into mobile interventions is especially relevant given a new rule from the Drug Enforcement Agency that will allow Opioid Treatment Programs to establish and operate mobile methadone vans without obtaining a separate DEA registration for each mobile component.
- For policy makers: Findings from this study suggest that a mobile engagement unit targeting at-risk areas and individuals may be a promising strategy to initiate methadone treatment among individuals with an opioid use disorder and may improve subsequent treatment utilization. Linking people to medication treatment before a crisis is a crucial component to solving the opioid crisis, as most individuals with opioid use disorder are not treated with these medications despite strong evidence for reducing mortality and improving other treatment outcomes. Implementing innovative interventions like this one along with providing additional funding to evaluate these interventions are critical in addressing this treatment gap. Many interventions that link people to treatment involve intervening shortly after an overdose, making mobile units especially desirable given that this is not a prerequisite to the intervention.
CITATIONS
Stewart, R.E., Shen, L., Kwon, N., Vigderman, J., Kramer, S., Mandell, D.S., Candon, M., Lamb, R., & Rothbard, A.B. (2021). Transporting to treatment: Evaluating the effectiveness of a mobile engagement unit. Journal of Substance Abuse Treatment, 129, 108377. doi:10.1016/j.jsat.2021.108377

