Stigmatization & Other Predictors of Addiction
Series: Breaking the Stigma
Previous studies have examined predictors of specific substance use and misuse, but there is a lack of studies examining predictors of alcohol and drug dependence itself.
This is important because dependence is more strongly associated with premature mortality and more disease and disability than substance use, and can have life-long ramifications. Consequently, investigation of factors that influence this specific risk are important to know.
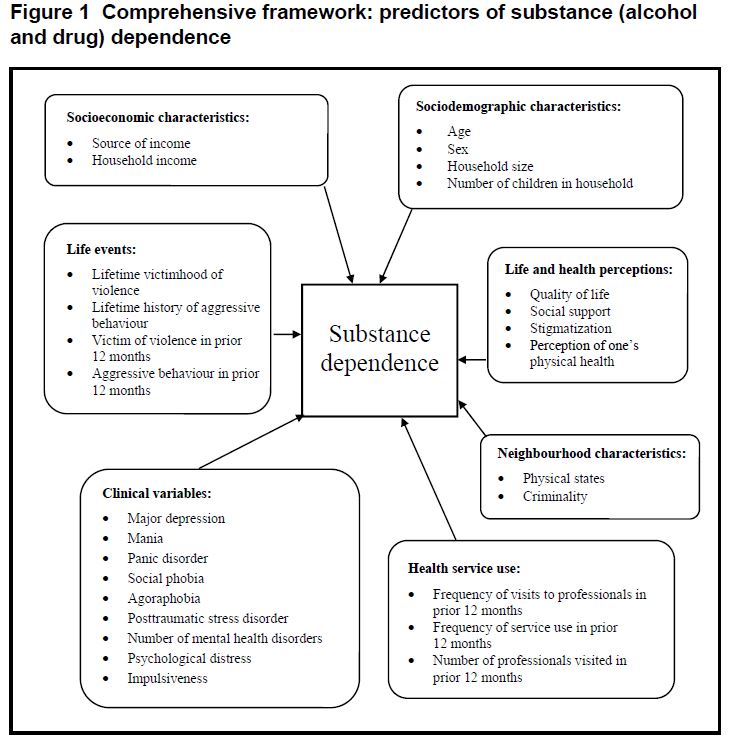
To identify new cases of dependence, Fleury and colleagues used longitudinal methods to find participants who developed substance dependence between the baseline interview and follow-up two years later. The authors were then able to identify predictors of incident substance use disorder from a variety of domains including socioeconomic characteristics (e.g., household income), life and health perceptions (e.g., quality of life, stigmatization), neighborhood characteristics (e.g., criminality), and health service use (e.g., frequency of visits).
The study population consisted of a representative sample of individuals ages 15 to 65 from Montreal, Canada. Of 2,434 people completing the baseline survey, 611 (25.1%) were lost to follow-up and thus were not able to be reassessed. The prevalence of substance dependence was 5.9% at time 1 and 3.7% at time 2. About 1.5% of participants had persistent substance dependence between the two time points. At time 2, 39 new cases of substance dependence were identified, representing 2.2% of the 1,741 individuals used in the analysis.
Source: (Fleury et al., 2014)
From the sample of 1741 participants, 64% were female, and the average age was 43 years.
Notably from the study:
- Participants with new cases of substance dependence vs. those without substance dependence were significantly more likely to be male (62% vs. 36%), younger (37 vs. 43 years old on average), and have a diagnosis of major depressive disorder in the past 12 months (18% vs. 8%).
- People who developed substance dependence were also more likely to have higher average psychological distress, impulsiveness, and stigmatization scores, and have lower quality of life scores than those who did not develop substance dependence.
- Those with substance dependence were significantly more likely to live in areas with better physical conditions than those without substance dependence.
The authors then used multiple logistic regression to determine which variables were predictors of incident substance dependence diagnosis. Male sex (odds ratio [OR]: 2.91), age (OR: 0.96), stigmatization score ≥2.5 (OR: 5.27), and impulsiveness score (OR: 1.06) were significant predictors of substance dependence. For example, the odds of developing substance dependence between time points 1 and 2 were 2.91 times higher for males than females.
The authors also found the following significant interactions: females with substance dependence were more likely to suffer from social phobia than males, older participants with substance dependence had lower income than younger participants, and younger participants with substance dependence had stronger social support than their older counterparts.
IN CONTEXT
In this study, the strongest predictor of substance dependence was stigmatization (determined by the Devaluation Discrimination scale, comprised of 12 questions with a 6-point Likert scale) such that those with a higher stigmatization score were 5.27 times more likely to develop a substance dependence than those with a lower score.
Since stigma can act as a barrier to treatment, health service utilization is an important variable to explore.
Although there are several nuances here, including aggregating participants from four separate studies, this study is an important addition to the adolescent treatment/recovery literature in understanding unique clinical profiles and needs.
- LIMITATIONS
-
- Only 2.5% of newly diagnosed participants reported health care service utilization for mental reasons in the past 12 months. Little more information was included in the study possibly due to the small sample size and low prevalence of substance dependence in the general population which made it difficult to capture a large amount of new cases.
- The study found that the 12-month prevalence of SUD was slightly higher at both time points than previous estimates from Canada which may suggest higher prevalence of SUD in this catchment area compared to the general population.
NEXT STEPS
A cohort study with more frequent follow-up intervals may be more appropriate for research questions exploring incident cases of substance use disorder (SUD) as it would allow for a longer time period in which participants can experience the endpoint (i.e., development of a SUD).
BOTTOM LINE
- For individuals & families seeking recovery: Seek professional help for addiction. It is not uncommon for people to wait years before getting help, but better outcomes can be achieved by intervening early.
- For scientists: Longer longitudinal studies with more frequent assessment time points and/or larger sample sizes are needed to fully address research questions pertaining to the development of SUDs.
- For policy makers: This study pointed toward an association between stigma and SUDs. This becomes a policy issue when stigmatization of the condition prevents individuals from receiving the help they need. Public health interventions are needed to address this stigma.
- For treatment professionals and treatment systems: Identifying predictors of SUDs can help tailor interventions to specific audiences. For example, since younger males were more likely to develop SUD, prevention methods can focus more specifically on this particularly vulnerable subgroup.
CITATIONS
Fleury, M. J., Grenier, G., Bamvita, J. M., Perreault, M., & Caron, J. (2014). Predictors of alcohol and drug dependence. Can J Psychiatry, 59(4), 203-212.

