Bang for your buck: Does addressing substance use problems in primary care decrease acute care expenses?
Detecting and addressing substance use disorder (SUD) in primary care settings, while not yet mainstream, may have distinct advantages. Most notable among these is the potential to reduce worsening of SUD symptoms for patients that could otherwise result in more intensive and expensive acute care service use. Despite this, few studies have examined this question. This study did just that and found that incorporating multifaceted SUD services into primary care led to less use of intensive services.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Measuring the real-life impact of new healthcare approaches is often challenging, no less so in the area of substance use disorder (SUD) treatment. One relevant metric, however, can be measured: healthcare utilization. Healthcare utilization has a direct impact on both patients and healthcare systems. For both, it is advantageous to reduce the number of acute and emergency care visits, so long as clinical care is delivered equally well in non-acute care settings, and, clinically, outcomes are maintained or improved. For patients, a reduction in acute care visits likely reflects a decreased occurrence of dangerous and life-threatening events (e.g., overdose, car crashes) that require more intensive services, and a shift towards less intensive outpatient services where treatment can be provided to potentially prevent the occurrence of events that would require more expensive care in the first place. For healthcare systems and those paying into them, a reduction of less intensive acute and emergency care visits represents cost savings.
Past research has indicated that incorporating SUD medications and related medical support into primary care can improve clinical outcomes. For example, initiation of buprenorphine treatment during medical hospitalizations and linkage to office-based buprenorphine treatment has been shown to be an effective means for engaging patients who are not seeking addiction treatment and for reducing illicit opioid use 6 months after hospitalization. Initiating buprenorphine treatment during emergency department visits has been shown to increase engagement in addiction treatment and to reduce (self-reported) illicit opioid use. Less is known regarding the impact on healthcare utilization. Some data exist that demonstrate that offering pharmacotherapy in primary care settings can reduce inpatient and emergency department utilization in patients with opioid and alcohol use disorder. Beyond pharmacotherapy, however, there are also other methods that might improve patient care for those presenting with SUD symptoms, including, for example, the use of recovery coaches, who are peers with a history of SUD who can offer outreach, treatment system navigation, and support for patients with SUD. To describe the impact of a multifaceted approach to SUD treatment in primary care, this study examined healthcare utilization data from one hospital network, in which some clinics used a multimodal strategy to provide SUD treatment within primary care, while other primary care clinics provided only referral to addiction services.
HOW WAS THIS STUDY CONDUCTED?
This study was a retrospective cohort analysis of administrative data, which means that it examined existing administrative records of a specifically-defined group of patients to describe their healthcare utilization over a specific period of time. In this case, the population being examined were primary care patients with an SUD diagnosis at 18 clinics within one hospital network. In order to compare the impact of the multimodal integrated care strategy, two types of clinics were compared. The first, clinics launching the integrated care model (4 clinics) consisting of the formation of interdisciplinary teams of local champions, access to pharmacotherapy with buprenorphine and extended-release naltrexone, counseling, and recovery coaching. This is compared to control clinics (14 clinics) that could offer referral to a standalone addiction treatment clinic offering pharmacotherapy and behavioral interventions. Included in analyses were adult patients with an SUD diagnosis receiving primary care at any of these 18 clinics. Since the study design was retrospective and naturalistic, steps were taken to strengthen the comparability of the patients seen at the two types of clinics so that study authors could attribute any potential advantage for integrated care to the multimodal treatment itself and not to characteristics of the patients who received integrated care.
To do this, healthcare utilization of patients receiving care at the integrated care clinics during the 9-month period prior to the launch of the integrated care program at that specific clinic was calculated, as was their healthcare utilization during the same 9-month period one year later (e.g., Jan-Sept 2014 compared to Jan-Sept 2015). The same healthcare utilization rates were calculated for patients receiving care at the more numerous control clinics, but only a small portion of these patients were included in analysis; namely, those patients matching most closely the characteristics of patients receiving care at the integrated care clinics. Specifically, matching was done based on age, sex, race, education level, level of medical comorbidities, type of SUD, and timing of SUD diagnosis. Out of a total of 1,868 integrated care patients and 5,135 control patients, a total of 1,353 pairs could be matched on these characteristics. These pairs were then compared on the outcomes of interest, namely the use of more intensive services. These included the number of inpatient admissions, length of inpatient stay, number of emergency department visits, as well as the number of primary care visits.
WHAT DID THIS STUDY FIND?
The matched pairs of patients were on average 49 years old, 60% male, 92% White, and primarily diagnosed with opioid (44%) and alcohol (37%) use disorder, or not otherwise specified (68%). As expected, during the 9-month follow-up period, patients receiving primary care at integrated care clinics spent fewer days in inpatient care (7.3 fewer days on average per 100 patients) and had fewer ED visits (6.7 fewer visits on average per 100 patients). Also as expected, patients receiving primary care at integrated care clinics had more primary care visits (9 more visits per 100 patients). Unexpectedly, the number of inpatient admissions were comparable between these two groups of patients.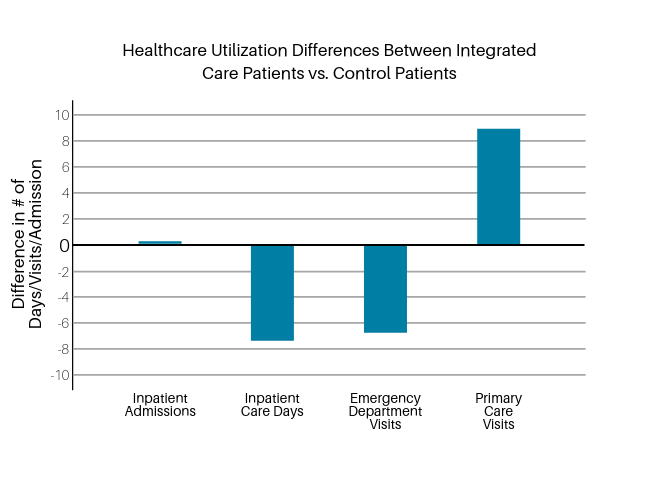
Figure 1. Differences in healthcare utilization between patients seen at integrated care versus control clinics during the 9-month follow-up period. Differences between patients seen at integrated care vs. control clinics are graphed for the 9-month period following the establishment of the integrated care clinics. Values represent differences in terms of number of admissions (inpatient admission), days in care (inpatient care), and number of visits per 100 patients (ED visits, primary care visits).
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
The model described in this paper, in which existing primary care patients are provided with access to SUD intervention approaches within their primary care setting, is a new model that is distinctly different in terms of its reach from previous approaches tested in large-scale, well-known clinical trials. Namely, in the AHEAD trial and the LINKAGE trial, individuals with SUD were recruited from SUD clinics (detox programs, outpatient programs), and provided with the opportunity and specific linkage to engage in primary care. The targeted outcomes of these two studies were different than in the current study. Instead of targeting decreased use of intensive services, the AHEAD trial sought to improve abstinence from stimulants, opioids, and heavy drinking, and the LINKAGE trial sought to improve patient activation and engagement in health care (increased login days and electronic patient portal use). By contrast, the multimodal approach described in this current study targeted already existing primary care patients in order to address their SUD and reduce further use of more intensive and expensive acute care services. Undoubtedly, this approach fails to reach many individuals with SUD who are not actively engaged in primary care, but it does address the problem of reducing the costs of treatment due to intensive service use while providing state-of-the-art SUD treatment.
The findings from this large retrospective cohort analysis of administrative data from one hospital network launching a new multimodal model of integrated care further strengthen the evidence base suggesting that providing SUD care within primary care systems may lower more intensive acute care utilization.
Due to the naturalistic approach of this study, it remains unclear which parts of the multimodal integrated care approach were the most effective. Previous research has demonstrated the effectiveness of pharmacotherapy provided in primary care to reduce the utilization of acute care. It is possible that the effects observed in this study are entirely due to this effect, rather than the additional impact of recovery coaches and the use of interdisciplinary teams of local champions, especially given that integrated care patients received more pharmacotherapy. On the other hand, it is quite likely that recovery coaches and interdisciplinary teams of local champions may have helped engage patients in initiating and maintaining pharmacotherapy, or that the observed decrease in acute care is attributable to other recovery support resources. Understanding which specific aspects of this multimodal approach are essential to have and which ones are not has the potential to save further on healthcare costs and add greater efficiency. This an important area for future research.
Meanwhile, the model described in this paper provides a working example of integrated care using multiple approaches and levels of integration, which may serve as a rich resource to consider for hospital networks seeking to improve ways in which they can better address SUD within primary care.
- LIMITATIONS
-
- Due to the naturalistic setting of this study, the compared groups were not randomized. Thus, it is possible that the clinics and the clinics’ patients may have been different in other ways that were not accounted for in this matched analysis.
- It is possible that patients in either group received care elsewhere, which would not have been captured in the healthcare utilization rates reported in this paper, which was restricted, by necessity, to data within the described hospital network.
- The hospital network used in this study was a well-established urban academic medical center. Generalizations to less well-resourced hospital networks should be made cautiously. Also, patients within this hospital network were predominantly White (92%), which limits generalizability to other racial/ethnic groups.
- It is not clear how transferrable the described model is to other settings. Rural settings, for example, may not have the personnel to pull together the resources to implement this treatment package.
BOTTOM LINE
This large retrospective cohort analysis of administrative data from one hospital network launching a new multimodal model of integrated care showed that patients receiving primary care at integrated care clinics spent fewer days in inpatient care, and had fewer ED visits, while engaging more in primary care. Unexpectedly, the number of inpatient admissions were comparable between these two groups of patients.
- For individuals and families seeking recovery: Increasingly, healthcare systems are taking a more integrative and preventive perspective on addressing harmful alcohol and drug use. Talking with your primary care providers about your substance use can be useful, as they can provide guidance, linkage and even initiation of SUD treatment, and thus may prevent you from experiencing dangerous and costly substance-related harm.
- For treatment professionals and treatment systems: Your hospital network may not have the type of integrated care clinics described in this paper, but addressing substance use disorder in primary care is increasingly becoming a standard for good practice. Strengthening the network connections between your addiction specialists and primary care providers and helping identify good linkage opportunities for patients is likely to benefit those patients and increase the efficiency of your healthcare system.
- For scientists: This paper is one of the first studies to look at the impact of recovery coaches on supporting patients with substance use disorder. Due to the multimodal nature of the integrated care model described, and the need to evaluate it in a real-life setting, this study could not isolate the effect of recovery coaches. Research is needed to better capture their impact in order to inform the clinical and public health utility of providing recovery coaching in primary care settings.
- For policy makers: Funding initiatives to address substance use disorder in a primary care setting are important and allow for the integrated treatment of physical and mental health. Just as important is funding that allows for systematic evaluation of such initiatives. Given that healthcare is such a major expense at local, state, and national levels, facilitating the building of a cumulative evidence base that can guide hospital administrators in choosing the most cost-effective practice is likely to be a sound investment.
CITATIONS
Wakeman, S. E., Rigotti, N. A., Chang, Y., Herman, G. E., Erwin, A., Regan, S., & Metlay, J. P. (2019). Effect of integrating substance use disorder treatment into primary care on inpatient and emergency department utilization. Journal of General Internal Medicine, 34(6), 871-877. doi: 10.1007/s11606-018-4807-x

