The Pain Drove Me To It
Opioid use disorder seems to be driven by physical or psychological pain as often as it is driven by a vulnerability to recreational opioid use. Those who began using primarily for the treatment of pain, however, view themselves as fundamentally different from recreational users which creates important barriers to care.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Given the growing prevalence of opioid use disorders over the past decade, and their continued rise despite efforts to prevent prescription misuse, it is important to accurately understand which pathways different individuals take that can result in problematic opioid use. There are scant prospective data documenting how individuals develop opioid use disorders, so we are limited to retrospective analyses. Understanding the pathways taken to opioid use disorders may shed light on possible routes rarely considered, so that efforts to prevent harmful opioid use might be enhanced and treatments might be tailored to greater effect.
HOW WAS THIS STUDY CONDUCTED?
The qualitative analysis presented in this study is derived from a larger mixed-methods study, the Treatment Options Study, focused on understanding the adoption of buprenorphine (typically referred to by its brand name Suboxone) medication-assisted treatment for opioid use disorders.
- MORE ON STUDY METHODS
-
The study subjects were drawn from the electronic medical records of the Kaiser-Permanente medical systems in the Northwest and Northern California.
In this study, adults with a minimum of two opioid use disorder diagnoses in the medical record were sent recruitment letters, resulting in 283 patients who were then brought in for one hour-long face-to-face semi-structured interviews. The questions were focused on addiction treatment, details of substance use and current and past pain.
Of the 283 patients, only 121 individuals included information about their pathway to opioid use disorders in the open-ended portion of the interview, and this analysis is focused on this latter group. These 121 open-ended descriptions of pathways taken to opioid use were coded with subsequent sub-theme coding, (ie there was no a priori hypotheses used to generate the categories).
Lastly, the group spontaneously referring to their pathway to opioid use disorder (n=121) was compared to the group not mentioning their pathway to misuse (n=162).
WHAT DID THIS STUDY FIND?
1. Five pathways to opioid use disorder emerged from spontaneous open-ended interviews: The responses from the 121 subjects in this sub-analysis fell into the following five pathways:
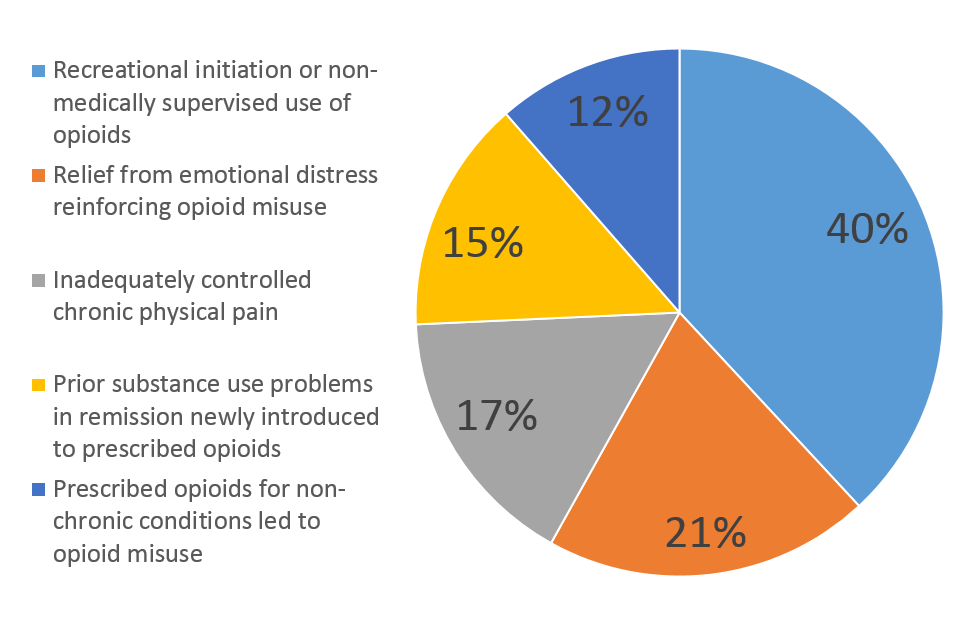
2. The different pain pathways, taken together, account for as large a percentage (50%) of new opioid use disorder as recreational use and prior substance use vulnerabilities combined.
3. Opioids used as antidepressants? Relief of emotional distress by opioids is anecdotally perceived by some to have an antidepressant or energizing effect (different from the dissociated high typically associated with opioid misuse) that also reinforces use and requires escalating doses to maintain this effect.
4. Fear of uncontrolled pain inhibits efforts to seek addiction treatment or reduce opioid use
5. Identifying as a pain patient may interfere with identifying as having a substance use disorder: The participants who were first treated for pain and then developed an opioid use disorder view themselves anecdotally in a different category as others with a similar opioid use disorder, acting as a further barrier to participating in substance use disorder treatment. When participating in treatment, they often focus on the differences between themselves and the others in treatment, thus potentially decreasing the effectiveness of treatment.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Pain, both physical and psychological, is a driver of opioid misuse and is simultaneously a barrier to treatment given concerns that the pain will not be adequately addressed once the opioids are stopped. Pain patients do not identify with broader opioid use disorder patients and may benefit from specialized substance use treatment focused on those primarily using opioids for pain.
Furthermore, relief of emotional distress may reinforce misuse (there is increasing research on the antidepressant effect of some of the opiate receptor pathways) and may explain in part the increased risk of opioid misuse among those with mental health diagnoses. Thus screening for prior substance use vulnerabilities and prior mental health struggles is strongly recommended prior to the initiation of opioid prescriptions.
- LIMITATIONS
-
- The interviews from which the data are collected did not directly ask about pathways to opioid use disorders – the pathways were inferred from the information offered in the open-ended portion of the interview. Furthermore, the study focused on less than half of the participants in the larger study, those that spontaneously provided enough information to infer a pathway to opioid use.
- The diagnosis of opioid use disorder was determined by chart review, and was not confirmed by a structured interview -a more reliable diagnostic tool
- This study only includes participants with a diagnosed opioid use disorder so the data cannot be used to understand factors protective for developing an opioid use disorder after opioids are prescribed for pain
- This is a retrospective study based on self-report, giving it the limited scientific rigor of a case series. The study nonetheless identifies areas meriting further research.
BOTTOM LINE
- For individuals & families seeking recovery: Identifying primarily as a pain patient may represent a significant barrier to benefiting from traditional opioid use disorder treatment. Anyone with a substance use disorder or a vulnerability to one should discuss this openly with prescribers prior to obtaining a prescription for opioids.
- For scientists: There is a need for prospective studies on the development of opioid use disorders where exposure to opioid prescriptions is documented so that the characteristics of those who go on to develop opioid use disorders can be identified.
- For policy makers: Creating pathways to opioid use disorder treatments that go hand-in-hand with pain control will reduce a significant barrier to treatment for those who continue to be dependent on opioids for pain despite developing an opioid use disorder. This will require the creation of a new modality of substance use disorder treatment, perhaps in collaboration with more recently developed pain clinics.
- For treatment professionals and treatment systems: Taking time to understand the initial pathway into an individual’s opioid use disorder will help identify the underlying issues that should be addressed directly during their substance use treatment (underlying vulnerability to substance use vs physical pain vs psychological pain, for instance) to help resolve the underlying driver of the opioid misuse.
CITATIONS
Stumbo, S. P., Yarborough, B. J. H., McCarty, D., Weisner, C., & Green, C. A. (2017). Patient-reported pathways to opioid use disorders and pain-related barriers to treatment engagement. Journal of substance abuse treatment, 73, 47-54.

