What is Happening in the Brains of Individuals with Cocaine Use Disorder Who Choose Money Over Drugs?
Overvaluing smaller-immediate rewards over larger-later rewards, know as “delay discounting” or “temporal discounting”, is one of the hallmark behaviors of individuals with substance use disorder.
Although there is a substantial body of research showing that delayed discounting is a strong predictor for who has (or will develop) substance use disorder, the field has only begun to examine optimal ways to leverage this crucial behavioral marker to enhance treatment and recovery.
In this cross-disciplinary study involving both self-report and functional magnetic resonance imaging (fMRI), Wesley and colleagues investigated differences between 25 individuals with cocaine “addiction” (meeting 5 of 7 criteria in DSM-IV, rather than the clinical 3 of 7 cutoff for dependence) and 25 without cocaine addiction (controls).
On average the individuals with cocaine use disorder used 24 days in the month leading up to study participation and had been using for 15 years. In the study, temporal discounting tasks took four forms each of which involved hypothetical “commodities”. Participants chose between less money now versus more money later and less cocaine now versus more cocaine later as well as between cocaine now and money later, and money now versus cocaine later.
Most relevant to treatment and recovery is the choice between cocaine now and money later, because this is among the most critical decisions faced by those in recovery:
Should I use now, and receive an immediate, predictable, and often powerful reward, while it might very well cost me in the future?
Or should I say no, perhaps use a recovery coping strategy, which will not feel as good in the immediate, but will allow me to save money, continue to make efforts toward recovery goals?
For those without substance use disorder (SUD), this decision is not a difficult one. Indeed, only 8% of controls chose cocaine now versus money later. Interestingly though, 50% of those with cocaine addiction chose future money over cocaine, suggesting if the future reward is large enough and meaningful, individuals with chronic cocaine use disorder will make the “healthy”, recovery-consistent choice. It is worth noting that, consistent with prior work, individuals with chronic cocaine use disorder users demonstrated a greater likelihood of choosing smaller immediate rewards over larger later rewards relative to controls.
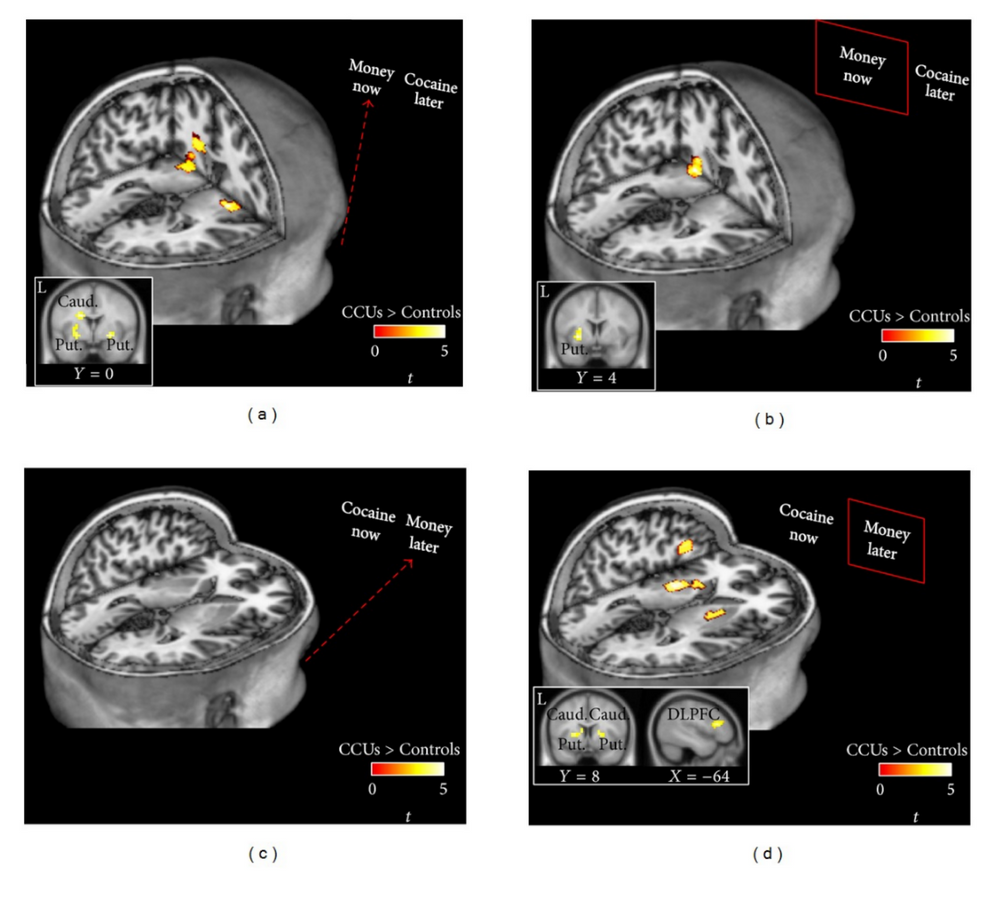
While they conducted many analyses, authors’ primary interest was to examine brain activity with fMRI during instances where the individuals with chronic cocaine use disorder chose future monetary reward.
Source: (Wesley et al., 2014)
Several prior studies have implicated the dorsal striatum in the formation of habits, and dopamine levels (the neurotransmitter most associated with pleasant emotional experience) in this area are strongly associated with drug craving.
Many scientists, however, posit that dampening the influence of the dorsal striatum would decrease relapse risk (and enhance recovery), though Wesley et al. found increased activity in this area to be associated with choosing money over cocaine, understood here as a recovery-seeking behavior.
The DLPFC is implicated in a collection of cognitive abilities known as executive functioning, characterized by tasks like planning, sequencing, organization, inhibiting impulses, and attention. Importantly, though perhaps not surprisingly, individuals with chronic cocaine use disorder choosing money over drugs showed increased activity in this region, consistent with prior results showing the area is associated with cost/benefit analyses.
IN CONTEXT
Despite the availability of many helpful evidence-based psychosocial and pharmacological treatments, novel approaches are needed to enhance the chances of recovery.
In this compelling study, Wesley and colleagues showed not only can individuals with severe cocaine use disorder choose money over cocaine about half the time, but that the dorsal striatum and dorsolateral prefrontal cortex appear to be implicated in these decisions.
As authors point out, these data highlight the role of both executive (frontal) functioning and emotional (limbic) processing in recovery from substance use disorders. These areas may serve as targets of future SUD treatments and recovery management approaches.
For example, strategies that encourage those in early recovery to anticipate negative consequences of use (sometimes referred to as “playing the tape all the way through”), as well as to identify and manage emotional triggers could maximize benefit from contingency management approaches that provide rewards for recovery behaviors like negative toxicology screens.
- LIMITATIONS
-
The sample excluded individuals with non-cocaine substance use disorder (SUD) apart from nicotine) as well as those with co-occurring psychiatric disorders. Given that at least 25-30% (conservatively) of SUD treatment patients meet for a co-occurring psychiatric disorder and approximately 50% use two or more substances upon entering treatment, we should be cautious in generalizing to substance use disorder patients at large.
CITATIONS
Wesley, M. J., Lohrenz, T., Koffarnus, M. N., McClure, S. M., De La Garza, R., Salas, R., … & Montague, P. R. (2014). Choosing money over drugs: the neural underpinnings of difficult choice in chronic cocaine users. Journal of addiction, 2014.

